In the quiet corners of our minds, where shadows often lurk unnoticed, clinical depression weaves a complex tapestry of emotions that can engulf even the brightest of spirits. It is a condition that transcends the fleeting sadness we all experience from time to time, manifesting as a profound and persistent sense of despair that can alter the very fabric of daily life. Unlike the typical fluctuations of mood, clinical depression is a labyrinthine illness, marked by a myriad of symptoms that can range from lethargy and apathy to overwhelming feelings of worthlessness. Understanding this intricate disorder is essential, not only for those who battle it but also for the loved ones who wish to support them. In this article, we will explore the nature of clinical depression, its symptoms, causes, and avenues for treatment, shedding light on a condition that remains all too often shrouded in misunderstanding and stigma.
Understanding the Spectrum of Clinical Depression
Clinical depression is far from a monolithic experience; it exists along a spectrum that captures a wide array of symptoms and intensities. Individuals may find themselves experiencing a variety of manifestations, ranging from persistent sadness and fatigue to anxiety and irritability. The severity of these symptoms can vary significantly, influencing daily functioning and overall quality of life. Some might navigate life with a constant, low-grade despair, while others may encounter more acute episodes that render them unable to carry out everyday tasks. Understanding the nuances of these experiences is crucial for both those affected and their support systems.
Several key factors contribute to the spectrum of clinical depression, including biological, psychological, and environmental influences. These factors can interact in complex ways, leading to a diverse range of depressive experiences. Below is a table highlighting some common types of depression, their characteristics, and typical treatment options:
| Type of Depression | Characteristics | Treatment Options |
|---|---|---|
| Major Depressive Disorder | Severe symptoms impacting daily life | Antidepressants, Therapy |
| Persistent Depressive Disorder | Chronic low mood lasting for years | Long-term therapy, Medication |
| Seasonal Affective Disorder | Depressive episodes triggered by seasons | Light therapy, Antidepressants |
| Psychotic Depression | Depression accompanied by hallucinations | Medication, Hospitalization |
Identifying Symptoms and Their Impact on Daily Life
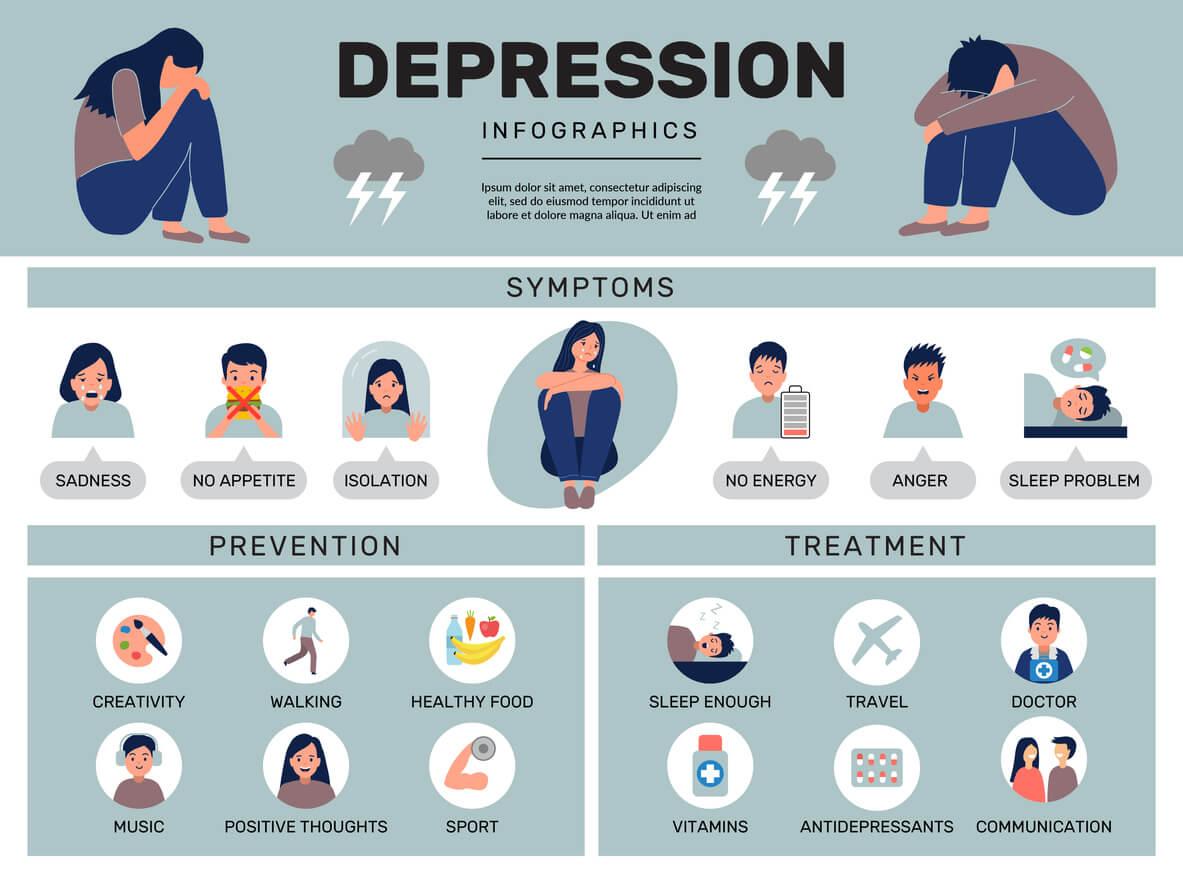
Clinical depression manifests through a spectrum of symptoms that can profoundly disrupt one’s daily life. Individuals may experience overwhelming feelings of sadness, hopelessness, and a lack of interest in activities that once brought joy. Other common symptoms include:
- Fatigue or low energy: Even simple tasks can feel insurmountable, leading to procrastination and frustration.
- Changes in appetite: Some may overeat to cope, while others might struggle to eat at all.
- Sleep disturbances: Insomnia or hypersomnia can lead to further exhaustion and irritability.
- Concentration difficulties: The ability to focus diminishes, affecting work and personal relationships.
The impact of these symptoms on daily life can be devastating. Relationships may suffer as the individual withdraws from social interactions, leading to isolation and loneliness. Work performance often declines, creating a cycle of stress and anxiety that exacerbates the symptoms. In many cases, those affected may find themselves unable to meet personal responsibilities, resulting in feelings of inadequacy and shame. Below is a table illustrating the correlation between symptoms and their effects on various aspects of life:
| Symptom | Impact on Life |
|---|---|
| Fatigue | Increased absenteeism from work. |
| Changes in Appetite | Weight fluctuations and related health issues. |
| Sleep Disturbances | Poor productivity and mood swings. |
| Concentration Difficulties | Struggles with decision-making and memory. |
Exploring Effective Treatment Options and Therapies
When it comes to addressing clinical depression, a multifaceted approach is often the most effective. Treatment options can vary widely, and it is essential for individuals to work closely with healthcare professionals to find a personalized plan that suits their unique needs. Some of the most common treatments include:
- Psychoeducation – Understanding the condition can empower individuals to manage their symptoms more effectively.
- Psychotherapy - Engaging in talk therapy, such as Cognitive Behavioral Therapy (CBT), can help change negative thought patterns.
- Medication – Antidepressants can be beneficial in balancing chemicals in the brain.
- Support Groups – Connecting with others facing similar struggles fosters a sense of community and shared understanding.
In addition to conventional therapies, some alternative treatments may provide relief for those suffering from clinical depression. These can include:
- Mindfulness and Meditation – Practices that encourage present-moment awareness can reduce stress and enhance emotional well-being.
- Exercise – Regular physical activity has been shown to boost mood and alleviate symptoms.
- Nutrition – A balanced diet rich in omega-3 fatty acids and whole grains can support brain health.
| Treatment | Effectiveness |
|---|---|
| Psychoeducation | High |
| Psychotherapy | Very High |
| Medication | Moderate to High |
| Alternative Therapies | Varies |
The Role of Lifestyle Changes in Managing Depression
Making intentional lifestyle changes can serve as a powerful adjunct to traditional treatment methods for clinical depression. By integrating healthy habits into daily routines, individuals can create an environment that supports emotional well-being. Consider the following strategies:
- Regular Exercise: Physical activity is known to release endorphins, which can boost mood and reduce feelings of sadness.
- Balanced Diet: Nutrition plays a vital role; a diet rich in vitamins, minerals, and omega-3 fatty acids can positively impact brain chemistry.
- Sleep Hygiene: Establishing a regular sleep schedule helps regulate mood and energy levels.
- Mindfulness Practices: Techniques such as meditation and yoga can reduce stress and enhance emotional resilience.
In addition to these changes, fostering strong social connections is essential in combating feelings of isolation that often accompany depression. Engaging with supportive friends or joining community groups can provide a sense of belonging and purpose. Below is a simple representation of how these elements interact:
| Lifestyle Change | Potential Benefits |
|---|---|
| Regular Exercise | Enhances mood, increases energy |
| Balanced Diet | Improves brain function, stabilizes energy |
| Sleep Hygiene | Regulates mood, boosts cognitive function |
| Mindfulness Practices | Reduces stress, improves emotional regulation |
| Social Connections | Fosters support, combats loneliness |
Building a Support System: The Importance of Connection
In times of clinical depression, forming and maintaining a strong support system can be a lifeline. Connections with others allow individuals to experience empathy, understanding, and a sense of belonging during their darkest moments. Engaging with friends, family, or support groups can help reduce feelings of isolation and provide a safe space to express emotions. Here are some key benefits of having a support system:
- Emotional Validation: Sharing experiences with someone who understands can validate feelings and help process emotions.
- Encouragement: Supportive individuals can inspire motivation to seek treatment and stick with it.
- Resource Sharing: Connections can lead to discovering helpful resources, such as therapists, support groups, or educational materials.
Building a network of trusted individuals can take time, but the rewards are invaluable. It’s essential to reach out and communicate openly, ensuring that those around you know how to support you best. Establishing this network doesn’t have to be overwhelming; it can start small and grow naturally over time. The following table highlights some potential sources of support:
| Type of Support | Examples |
|---|---|
| Personal | Friends, Family Members |
| Professional | Therapists, Counselors |
| Peer | Support Groups, Online Communities |
Strategies for Long-Term Recovery and Resilience
Building a foundation for sustained recovery from clinical depression involves engaging in a holistic approach that nurtures both mental and physical health. Regular physical activity can significantly enhance mood and reduce symptoms of depression, so consider incorporating exercises like brisk walking, yoga, or dancing into your routine. Mindfulness practices, such as meditation or deep-breathing exercises, can help center your thoughts and alleviate anxiety. Additionally, establishing a consistent sleep schedule is vital for emotional stability; aim for 7-9 hours of quality sleep each night. Don’t underestimate the power of social support—connect with friends, family, or support groups that understand your journey. These relationships provide a safety net and a sense of belonging, which are crucial during recovery.
Incorporating nutritious foods into your diet can also positively influence your mood and energy levels. A balanced diet rich in fruits, vegetables, whole grains, and omega-3 fatty acids can play a pivotal role in brain health. Consider keeping a wellness journal to track your feelings, triggers, and progress, which can offer insights and help reinforce positive changes in your life. The process of recovery is often non-linear, so be patient with yourself and recognize that setbacks are part of the journey. Setting realistic goals and celebrating small victories can instill a sense of achievement and motivate you to continue on the path toward resilience. Remember, each step, no matter how small, contributes to your overall well-being.
Q&A
Q&A: Understanding Clinical Depression
Q1: What is clinical depression?
A1: Clinical depression, often referred to as major depressive disorder (MDD), is a serious mental health condition that affects how a person feels, thinks, and handles daily activities. Unlike the fleeting sadness that everyone experiences, clinical depression persists for weeks or longer, significantly impacting one’s quality of life.
Q2: What are the symptoms of clinical depression?
A2: Symptoms of clinical depression vary widely but commonly include persistent feelings of sadness or hopelessness, a loss of interest in activities once enjoyed, changes in appetite or weight, sleep disturbances, fatigue, difficulty concentrating, feelings of worthlessness, and even thoughts of death or suicide. It’s essential to recognize these symptoms as more than just a temporary phase; they indicate a deeper psychological struggle.
Q3: How is clinical depression diagnosed?
A3: Diagnosis of clinical depression typically involves a comprehensive evaluation by a mental health professional. This may include a detailed discussion of the individual’s symptoms, medical history, and possibly standard questionnaires. There is no single test for depression; rather, it’s a combination of clinical assessments that lead to a diagnosis.
Q4: What causes clinical depression?
A4: The causes of clinical depression are complex and multifaceted, often involving a combination of genetic, biological, environmental, and psychological factors. Life events, such as trauma, loss, or prolonged stress, can trigger episodes of depression, especially in individuals with a predisposition to the disorder.
Q5: How is clinical depression treated?
A5: Treatment for clinical depression often includes a combination of psychotherapy, medication, and lifestyle changes. Psychotherapy, such as cognitive-behavioral therapy (CBT), can help individuals address negative thought patterns. Antidepressants can balance chemicals in the brain that affect mood. Additionally, lifestyle modifications like regular exercise, a healthy diet, and stress management techniques can support recovery.
Q6: Can clinical depression be prevented?
A6: While it may not always be possible to prevent clinical depression, certain strategies can reduce the risk. These include maintaining strong social connections, managing stress, engaging in regular physical activity, and seeking help when feeling overwhelmed. Early intervention and awareness can significantly improve outcomes for those at risk.
Q7: What should someone do if they think they have clinical depression?
A7: If someone suspects they have clinical depression, it’s crucial to seek help from a mental health professional. Reaching out can be the first step toward recovery. Support from friends and family is also invaluable during this time. Remember, acknowledging the need for help is a sign of strength, not weakness.
Q8: Is there hope for recovery from clinical depression?
A8: Absolutely. Many individuals with clinical depression find relief through proper treatment and support. While the journey to recovery can be challenging, many people go on to lead fulfilling lives. With the right strategies and support system in place, hope is very much alive.
This Q&A aims to shed light on the complexities of clinical depression while encouraging understanding and support for those affected.
Closing Remarks
In the intricate tapestry of human emotion, clinical depression stands as a thread that can darken the fabric of our lives, often weaving a narrative of struggle and resilience. As we draw the curtains on this exploration, it’s essential to recognize that while clinical depression casts a long shadow, it is not an insurmountable barrier. Understanding, compassion, and informed treatment can illuminate pathways to recovery, offering hope where despair may linger.
In our journey through the nuances of this condition, we’ve uncovered the importance of awareness—both in recognizing the signs within ourselves and in extending a hand to others who may be quietly battling their own storms. As we move forward, let us advocate for open dialogues, dispel stigmas, and foster environments where mental health is prioritized and understood.
Ultimately, clinical depression may be a chapter in many lives, but it does not define the entirety of one’s story. With ongoing research, community support, and a commitment to empathetic listening, we can transform this chapter into one of healing and renewal—a testament to the enduring strength of the human spirit. As we step into the light of tomorrow, may we carry with us the lessons learned and the hope ignited, forging a future where mental health is embraced as an integral part of our shared humanity.