Unraveling the Mystery of Celiac Disease: A Journey through Gluten Sensitivity
In a world where food frequently takes center stage, the rise of dietary restrictions has prompted many to reconsider what they consume. Among these conditions, celiac disease stands out as a complex and often misunderstood ailment that affects millions globally. It’s more than just a dislike of gluten; it’s an autoimmune disorder that triggers a profound reaction in the body, leading to a myriad of symptoms that can be debilitating. As we embark on this exploration of celiac disease, we will navigate its origins, the science behind its diagnosis, and the lifestyle adjustments required for those living with this condition. Join us as we shed light on the intricacies of celiac disease, separating myth from fact and offering insights into a path toward understanding and health.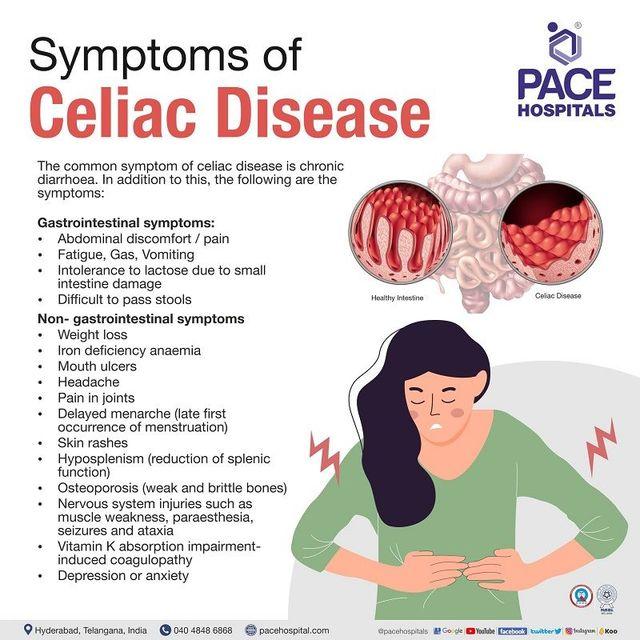
Understanding Celiac Disease: An Overview of Causes and Symptoms
Celiac disease is an autoimmune disorder triggered by the consumption of gluten, a protein found in wheat, barley, and rye. When individuals with this condition ingest gluten, their immune system responds abnormally, leading to inflammation and damage in the small intestine. This damage can disrupt nutrient absorption, resulting in a range of health issues. While the exact cause of celiac disease remains unclear, several factors contribute to its development, including:
- Genetic predisposition: A family history of celiac disease increases the likelihood of developing the condition.
- Environmental factors: Certain viral infections and changes in gut bacteria may play a role in triggering the disease.
- Timing of gluten introduction: Introducing gluten in early childhood may influence the risk, although this is still under investigation.
The symptoms of celiac disease can vary significantly from person to person, making it a challenging condition to diagnose. Some individuals may experience gastrointestinal issues, while others may present with non-digestive symptoms. Common symptoms include:
| Gastrointestinal Symptoms | Non-Gastrointestinal Symptoms |
|---|---|
| Abdominal pain | Fatigue |
| Diarrhea | Joint pain |
| Bloating | Skin rashes |
| Weight loss | Delayed growth in children |
Navigating a Gluten-Free Diet: Essential Foods and Alternatives
Living with celiac disease requires a careful selection of foods to ensure a healthy and balanced diet while avoiding gluten. Fortunately, a wide variety of gluten-free options are available to help you maintain your nutritional needs. Incorporating whole, unprocessed foods into your diet is crucial. Fruits, vegetables, lean meats, fish, eggs, dairy, and legumes are naturally gluten-free and can form the backbone of your meals. Additionally, gluten-free grains such as quinoa, brown rice, millet, and amaranth can add diversity and texture to your meals.
In addition to embracing naturally gluten-free foods, it’s essential to explore delicious alternatives to traditional gluten-containing staples. For example, you can swap out wheat flour for almond flour, coconut flour, or gluten-free blends when baking. Similarly, pasta can be replaced with zucchini noodles, rice noodles, or chickpea pasta for a satisfying gluten-free meal. To help you make informed choices, consider using the following table to compare gluten-free alternatives with their traditional counterparts:
| Traditional Food | Gluten-Free Alternative |
|---|---|
| Wheat Flour | Almond Flour |
| Bread | Gluten-Free Bread or Lettuce Wraps |
| Pasta | Chickpea Pasta or Zucchini Noodles |
| Beer | Gluten-Free Beer or Hard Seltzer |
The Importance of Diagnosis: Tests and Procedures for Celiac Disease
A precise diagnosis is crucial for individuals suspected of having celiac disease, as the condition can lead to severe long-term health complications if left untreated. The diagnostic journey typically begins with a thorough review of medical history and symptom assessment by a healthcare provider. Following this, a series of tests are conducted to confirm the presence of the disease. These tests include:
- Serological tests: Blood tests that measure specific antibodies; elevated levels often indicate celiac disease.
- Genetic testing: Analyzes genes related to celiac disease, helping to determine susceptibility.
- Endoscopy with biopsy: A procedure where a thin tube is inserted into the small intestine to collect tissue samples for examination.
Each of these tests plays a pivotal role in forming a comprehensive picture of the patient’s health. In many cases, initial serological tests will guide the need for further invasive procedures like endoscopy. Moreover, understanding the test results is essential for both patients and healthcare providers, as it can impact treatment decisions. Below is a simplified comparison of testing options:
| Test Type | Purpose | Procedure |
|---|---|---|
| Serological Tests | Detects antibodies in the blood | Blood sample analysis |
| Genetic Testing | Identifies genetic predisposition | DNA sample analysis |
| Endoscopy | Directly examines the small intestine | Invasive tissue sampling |
Managing Celiac Disease: Lifestyle Changes and Support Strategies
Living with celiac disease requires a significant adjustment to one’s daily routine, primarily focusing on a strict gluten-free diet. This transition involves not only avoiding obvious sources of gluten, such as wheat, barley, and rye, but also being vigilant about cross-contamination. To help navigate this lifestyle change, consider implementing the following strategies:
- Education: Understanding food labels and ingredients is crucial. Familiarize yourself with gluten-containing and gluten-free grains.
- Meal Planning: Prepare meals in advance to ensure gluten-free options are readily available.
- Cook at Home: Homemade meals allow for better control over ingredients and reduce the risk of contamination.
- Support Groups: Connecting with others who share similar experiences can provide emotional support and practical tips.
A comprehensive approach to managing celiac disease also includes regular consultations with healthcare professionals, such as dietitians who specialize in gluten-free diets. This support can help fine-tune your dietary choices and ensure nutritional adequacy. Additionally, consider keeping a food diary to track your symptoms and food intake. A simple table can assist in monitoring your progress:
| Date | Food Consumed | Symptoms Noted |
|---|---|---|
| MM/DD/YYYY | Gluten-free pasta with vegetables | No symptoms |
| MM/DD/YYYY | Quinoa salad | Minor bloating |
| MM/DD/YYYY | Rice and grilled chicken | No symptoms |
Common Myths and Misconceptions: Debunking Celiac Disease Myths
Celiac disease is often shrouded in misunderstanding, leading to several myths that can complicate the lives of those affected. One common misconception is that celiac disease is just a food allergy. In reality, celiac disease is an autoimmune disorder where the ingestion of gluten triggers an immune response that damages the small intestine. Unlike food allergies, which can cause immediate reactions, celiac disease can result in long-term health issues if gluten is consumed over time. Furthermore, many believe that individuals with celiac disease can tolerate small amounts of gluten; however, even minute traces can cause significant harm to their digestive system.
Another prevalent myth is that celiac disease is a fad or trend that can be outgrown. This misconception can lead to a lack of understanding and support for those diagnosed. Celiac disease is a lifelong condition that requires strict adherence to a gluten-free diet. It’s also important to note that gluten-free does not automatically mean healthy. Many gluten-free products are highly processed and may lack essential nutrients. To provide better insight, consider the following table highlighting common myths versus the facts:
| Myth | Fact |
|---|---|
| Celiac disease is a food allergy. | It is an autoimmune disorder. |
| People with celiac can eat small amounts of gluten. | Even tiny amounts can cause damage. |
| Celiac is just a trend. | It is a lifelong condition. |
| Gluten-free means healthy. | Gluten-free products can be unhealthy. |
The Role of Support Networks: Finding Community and Resources for Patients
For patients navigating the complexities of celiac disease, establishing a robust support network can be invaluable. Connecting with others who share similar experiences fosters a sense of belonging and understanding that can ease the emotional burden. Building these networks can involve:
- Local support groups: These provide a safe space for sharing experiences, recipes, and coping strategies.
- Online forums: Virtual communities offer 24/7 access to advice and emotional support, regardless of location.
- Social media groups: Engaging with others on platforms like Facebook or Instagram can help patients stay informed and inspired.
Moreover, tapping into available resources is crucial for managing the day-to-day challenges of living with celiac disease. Various organizations offer comprehensive information tailored for patients, including:
| Resource | Description |
|---|---|
| Celiac Disease Foundation | Provides education, advocacy, and research funding to improve the lives of those affected. |
| National Institutes of Health | Offers clinical guidelines and research findings to help patients and healthcare providers. |
| Gluten-Free Living Magazine | A publication filled with recipes, tips, and product reviews for gluten-free living. |
Q&A
Q&A on Celiac Disease: Understanding the Gluten-Free Journey
Q1: What is celiac disease?
A1: Celiac disease is an autoimmune disorder that occurs in genetically predisposed individuals, where the ingestion of gluten—a protein found in wheat, barley, and rye—triggers an immune response damaging the small intestine. This damage can lead to malabsorption of nutrients and a wide range of health issues.
Q2: What are the common symptoms of celiac disease?
A2: Symptoms can vary widely among individuals, but commonly include digestive issues such as diarrhea, bloating, and abdominal pain. Other symptoms might include fatigue, weight loss, anemia, joint pain, skin rashes, and neurological symptoms like headaches or cognitive disturbances. Some individuals may experience no symptoms at all, making diagnosis challenging.
Q3: How is celiac disease diagnosed?
A3: Diagnosis typically involves a combination of blood tests to check for specific antibodies and a biopsy of the small intestine to assess damage. It’s essential to continue consuming gluten before testing to ensure accurate results. If diagnosed, a strict, lifelong gluten-free diet is the only effective treatment.
Q4: Can celiac disease be treated or cured?
A4: Currently, there is no cure for celiac disease. The cornerstone of management is adherence to a gluten-free diet, which allows the intestines to heal and prevents further damage. With diligent dietary changes, most individuals can lead healthy, symptom-free lives.
Q5: What are some challenges faced by those with celiac disease?
A5: Individuals with celiac disease often encounter social and dietary challenges. Eating out can be daunting, as cross-contamination is a risk, and not all establishments are well-versed in gluten-free practices. Additionally, reading labels and understanding food ingredients requires vigilance and education, as gluten can hide in many unexpected products.
Q6: Are there any ongoing research efforts related to celiac disease?
A6: Yes! Researchers are actively investigating new treatments, including potential medications that could allow safe gluten consumption, therapies to promote intestinal healing, and improved methods of diagnosis. Studies on the microbiome’s role in celiac disease are also gaining traction, potentially unveiling new insights into the condition.
Q7: What does a gluten-free diet entail?
A7: A gluten-free diet excludes all sources of gluten, including obvious grains like wheat, barley, and rye, as well as products derived from them. However, it also includes a wide variety of naturally gluten-free foods such as fruits, vegetables, meat, dairy, and gluten-free grains like rice and quinoa. It’s essential to read labels carefully and choose certified gluten-free options whenever possible.
Q8: How can friends and family support someone with celiac disease?
A8: Support comes through understanding and respect for dietary restrictions. Learning about celiac disease, offering gluten-free options in social settings, and being mindful of cross-contamination are all ways friends and family can help. Encouraging open communication about food choices and being patient during adjustments can also foster a supportive environment.
Q9: Is there a community for individuals with celiac disease?
A9: Absolutely! Numerous organizations and online forums offer support, resources, and a sense of community for those living with celiac disease. These platforms can provide valuable information on navigating the gluten-free lifestyle, sharing recipes, and connecting with others who understand the challenges of the condition.
Q10: What final advice would you give to someone newly diagnosed with celiac disease?
A10: Embrace the journey! While the diagnosis may feel overwhelming at first, it opens a door to healthier eating habits and self-care. Educate yourself, seek support, and don’t hesitate to reach out to healthcare providers for guidance. With time and commitment, living gluten-free can become a rewarding lifestyle that promotes your overall well-being.
Future Outlook
navigating the complexities of celiac disease requires a blend of awareness, education, and lifestyle adjustments. For those living with this autoimmune condition, understanding the nuances of gluten and its implications on overall health is paramount. As research continues to unfold, it is hoped that advances in treatment and a deeper understanding of celiac disease will pave the way for improved quality of life. By fostering a supportive community and spreading accurate information, we can empower individuals with celiac disease to embrace their journeys with resilience and confidence. Remember, while the path may be challenging, it is one that can be traveled with informed choices and a proactive approach. Here’s to a future where gluten-free living is not just a necessity, but a celebration of health and well-being.
