In the intricate landscape of human health, the gastrointestinal system often commands our attention with its delicate balance and complex functions. Among the myriad conditions that can disrupt this harmony, diverticulitis emerges as a notable contender—an ailment that reflects both the resilience and vulnerability of our digestive tract. Characterized by inflammation of small pouches that can form in the walls of the colon, diverticulitis serves as a reminder of how our dietary choices and lifestyle can manifest in physical ailments. As we delve into the nuances of this condition, we will explore its causes, symptoms, and treatment options, shedding light on a topic that affects millions yet remains shrouded in misunderstanding. Whether you are seeking knowledge for yourself or to support a loved one, this exploration aims to demystify diverticulitis and empower you with insights for better health.
Understanding Diverticulitis: Causes and Symptoms
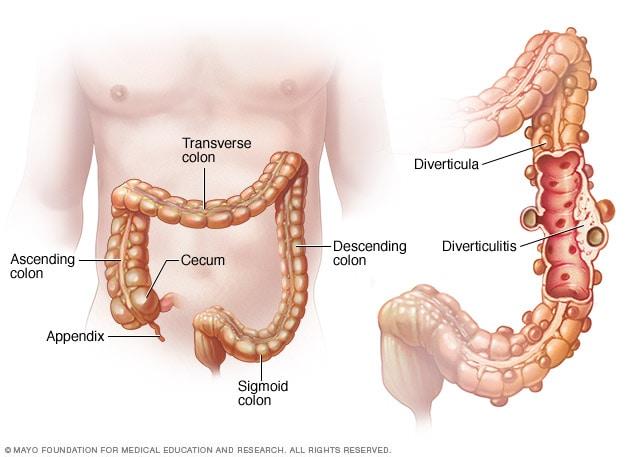
Diverticulitis arises when small pouches, known as diverticula, form in the wall of the colon and become inflamed or infected. This condition is more prevalent in individuals over 40 and may be influenced by a variety of factors, including a diet low in fiber, lack of physical activity, and obesity. Some key causes include:
- Dietary choices: Low fiber intake can lead to harder stools, increasing pressure in the colon.
- Age: The likelihood of developing diverticulitis increases with age.
- Genetics: A family history of diverticular disease may increase risk.
The symptoms of diverticulitis can range from mild to severe and often manifest suddenly. Common symptoms include:
- Abdominal pain: Typically localized to the lower left side.
- Fever: Often accompanied by chills.
- Digestive irregularities: Such as constipation or diarrhea.
In some cases, complications may arise, making it crucial to recognize the signs early. These complications can include abscesses, perforation of the colon, or even peritonitis, which requires immediate medical attention.
The Role of Diet in Managing Diverticulitis
Diet plays a crucial role in the management of diverticulitis, influencing both the onset of symptoms and overall digestive health. Many individuals with this condition are advised to focus on a high-fiber diet, which can help to soften stool and promote regular bowel movements. Incorporating a variety of fiber-rich foods can facilitate this process, including:
- Fruits: Apples, pears, and berries
- Vegetables: Broccoli, carrots, and spinach
- Whole grains: Oats, quinoa, and brown rice
- Legumes: Lentils, black beans, and chickpeas
In contrast, some individuals may need to temporarily reduce fiber intake during acute flare-ups to minimize bowel irritation. It’s essential to be mindful of certain foods that could exacerbate symptoms. Foods to watch out for include:
- Processed meats: Sausages and hot dogs
- High-fat dairy products: Cream and cheese
- Nuts and seeds: Although they’re healthy, they can be difficult to digest during a flare-up
Additionally, hydration is key. Drinking plenty of water can help fiber do its job effectively, preventing constipation and maintaining digestive health. Consulting with a healthcare professional or a nutritionist can provide tailored dietary recommendations that suit individual needs and conditions.
Lifestyle Changes to Reduce the Risk of Diverticulitis Flare-Ups
Making thoughtful lifestyle choices can significantly lower the chances of experiencing diverticulitis flare-ups. Dietary modifications play a crucial role in supporting digestive health. Emphasizing a diet rich in fiber can facilitate regular bowel movements and prevent the formation of diverticula. Consider incorporating:
- Fruits and Vegetables: Aim for a colorful variety, including berries, leafy greens, and carrots.
- Whole Grains: Swap refined grains for whole options like brown rice, oats, and whole wheat bread.
- Legumes: Beans and lentils are excellent sources of fiber and protein.
Hydration is equally important; drinking sufficient water helps fiber do its job effectively. In addition to dietary changes, adopting a few lifestyle habits can make a difference. Regular exercise can aid digestive health and promote regularity, while stress management techniques like meditation and yoga may also be beneficial. Avoiding smoking and limiting alcohol consumption can further reduce risk factors associated with diverticulitis. Consider this simple table as a quick reference for essential habits:
| Habit | Benefit |
|---|---|
| High Fiber Diet | Promotes regular bowel movements |
| Regular Exercise | Enhances digestive function |
| Hydration | Supports fiber digestion |
| Stress Management | Reduces gastrointestinal tension |
Medical Treatments and When to Seek Help
When it comes to managing diverticulitis, medical treatments vary based on the severity of the condition. For mild cases, a healthcare provider may recommend a clear liquid diet to allow the colon to heal. As symptoms improve, patients can gradually reintroduce low-fiber foods, eventually transitioning back to a high-fiber diet. Over-the-counter pain relievers may help alleviate discomfort, while antibiotics are often prescribed for more severe or recurrent infections. In some cases, dietary changes and lifestyle modifications, such as increased physical activity and hydration, play a crucial role in preventing further flare-ups.
However, it’s essential to recognize when professional medical intervention is necessary. Seek help if you experience any of the following symptoms:
- Severe abdominal pain that lasts for more than a few days
- High fever above 101°F (38.3°C)
- Persistent nausea or vomiting that prevents you from eating or drinking
- Rectal bleeding or changes in bowel habits
If conservative treatments fail or if complications arise such as abscesses or perforations, surgical options like a colectomy, which involves removing the affected portion of the colon, may be necessary. It’s important to consult with your healthcare provider to determine the best course of action tailored to your specific needs.
Long-Term Outlook: Living with Diverticulitis
Managing diverticulitis is often a lifelong journey that requires a careful balance of dietary choices, physical activity, and regular medical check-ups. Many individuals find that adopting a high-fiber diet plays a crucial role in minimizing flare-ups and promoting digestive health. Incorporating foods such as:
- Fruits and vegetables
- Whole grains
- Nuts and seeds
can significantly contribute to overall well-being. It’s important to gradually introduce fiber into your diet to avoid digestive distress, and staying hydrated is equally essential. Regular exercise not only aids digestion but also helps maintain a healthy weight, which can reduce the risk of complications associated with diverticulitis.
Furthermore, staying informed about your condition can empower you to make better lifestyle choices. Consider keeping a journal to track your symptoms and dietary habits, helping you to identify potential triggers. Regular consultations with your healthcare provider are vital, as they can provide tailored advice and monitor your situation closely. Here’s a simple overview of some recommended practices:
| Practice | Benefits |
|---|---|
| High-Fiber Diet | Promotes bowel health |
| Regular Exercise | Improves digestion, aids weight management |
| Hydration | Supports overall digestive function |
| Medical Check-ups | Ensures proper management of the condition |
Support and Resources for Patients and Caregivers
Living with diverticulitis can be challenging, not just for patients but also for their caregivers. Fortunately, there are numerous support and resources available to help navigate this journey. Some key resources include:
- Support Groups: Connecting with others who have similar experiences can provide emotional support and practical advice. Organizations like the Crohn’s & Colitis Foundation offer local and online support groups.
- Educational Materials: Websites such as Mayo Clinic and the National Institute of Diabetes and Digestive and Kidney Diseases provide extensive information about diverticulitis, including symptoms, treatment options, and dietary advice.
- Dietary Resources: Consulting a registered dietitian can help in creating a tailored eating plan that minimizes symptoms. Many hospitals and clinics offer nutrition counseling.
Additionally, having access to professional healthcare providers is crucial. Consider the following options:
| Type of Provider | Role |
|---|---|
| Gastroenterologist | Specializes in digestive health and can provide expert guidance on treatment. |
| Surgeon | May be necessary for severe cases requiring surgical intervention. |
| Primary Care Physician | Coordinates overall care and helps manage symptoms and medications. |
| Mental Health Counselor | Offers support for emotional challenges related to chronic health issues. |
By leveraging these resources, patients and caregivers can foster a supportive environment that promotes healing and well-being.
Q&A
Q&A on Diverticulitis: Understanding the Condition
Q: What exactly is diverticulitis?
A: Diverticulitis is an inflammation or infection of small pouches called diverticula that can form in the walls of the digestive tract, particularly in the colon. These pouches develop from a condition known as diverticulosis, where weak spots in the colon wall allow for bulging. When these pouches become inflamed or infected, it leads to diverticulitis.
Q: What causes diverticulitis?
A: While the exact cause of diverticulitis is not fully understood, factors such as a low-fiber diet, aging, and certain lifestyle habits may contribute to its development. When diverticula become blocked with food particles or bacteria, inflammation can occur, leading to an episode of diverticulitis.
Q: Who is at risk for developing diverticulitis?
A: Diverticulitis is more common in older adults, particularly those over the age of 40. Other risk factors include a sedentary lifestyle, obesity, smoking, and a diet low in fiber. Interestingly, it tends to be less common in populations that consume a high-fiber diet, such as those in developing countries.
Q: What are the symptoms of diverticulitis?
A: Common symptoms include abdominal pain (typically on the lower left side), fever, nausea, a change in bowel habits, and bloating. The pain can be sharp and may worsen with movement. In severe cases, complications like abscesses or perforations may arise, necessitating immediate medical attention.
Q: How is diverticulitis diagnosed?
A: Diagnosis often involves a combination of medical history, physical examination, and imaging tests, such as a CT scan or ultrasound. These methods help visualize the inflammation and rule out other conditions that may present similar symptoms.
Q: What treatment options are available for diverticulitis?
A: Treatment depends on the severity of the condition. Mild cases may be managed with dietary changes, such as a temporary low-fiber diet and antibiotics. More severe cases might require hospitalization and potentially surgery to remove the affected portion of the colon.
Q: Can diverticulitis be prevented?
A: While there is no guaranteed way to prevent diverticulitis, a high-fiber diet, regular physical activity, and adequate hydration can help reduce the risk. Incorporating plenty of fruits, vegetables, whole grains, and legumes into your diet is beneficial for overall digestive health.
Q: Is diverticulitis a lifelong condition?
A: Diverticulitis can recur, but many people manage it successfully with lifestyle changes and proper treatment. It’s important to monitor your symptoms and discuss any changes with your healthcare provider to ensure effective management.
Q: When should someone seek medical attention regarding diverticulitis?
A: You should seek medical attention if you experience severe abdominal pain, fever, or persistent changes in bowel habits, especially if these symptoms are new or worsening. Early intervention can help prevent complications and improve outcomes.
Q: Are there any long-term complications associated with diverticulitis?
A: Yes, potential long-term complications can include chronic abdominal pain, bowel obstruction, and in rare cases, the formation of fistulas. Regular follow-ups with a healthcare provider and adherence to treatment plans are essential for minimizing these risks.
This Q&A aims to provide a comprehensive understanding of diverticulitis, its causes, symptoms, and management, enabling readers to approach the subject with clarity and informed awareness.
Final Thoughts
In closing, diverticulitis serves as a poignant reminder of the delicate balance our digestive systems maintain. As we navigate the complexities of dietary choices and lifestyle habits, awareness and understanding become our allies in prevention and management. Whether you are experiencing the condition firsthand or supporting a loved one through it, knowledge empowers us to seek proactive measures and make informed decisions. Remember, every journey toward wellness begins with a single step—be it a visit to the doctor, a shift in eating habits, or simply staying educated about your health. In embracing these changes, we not only foster our own well-being but also contribute to a broader conversation about digestive health, resilience, and the human experience. As we bid adieu to this exploration of diverticulitis, let us carry forward the lessons learned and cultivate a future where our digestive health thrives.