In the delicate ecosystem of the human body, balance is key. Yet, when that harmony is disrupted, particularly in the intimate regions, discomfort can arise in the form of a yeast infection. This common ailment, often shrouded in stigma and misunderstanding, affects millions and can lead to a spectrum of symptoms that range from mild irritation to significant distress. Fortunately, the world of medicine offers a variety of treatments designed to restore that balance and alleviate suffering. In this article, we will explore the landscape of yeast infection medicine, delving into its causes, symptoms, and the range of treatment options available—empowering readers with the knowledge they need to reclaim their comfort and health.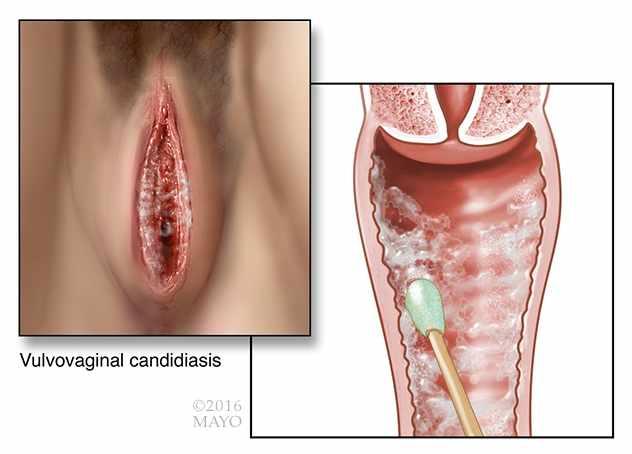
Understanding Yeast Infections and Their Causes
Yeast infections, primarily caused by the fungus Candida albicans, can occur in various parts of the body, most commonly in warm, moist areas such as the vagina, mouth, and skin folds. This opportunistic organism thrives in environments where the natural balance of bacteria and fungi has been disrupted. Contributing factors include:
- Antibiotic use: Disrupts the balance of healthy bacteria.
- Hormonal changes: Fluctuations during menstruation, pregnancy, or hormonal therapies can promote growth.
- Weakened immune system: Conditions like HIV/AIDS, diabetes, or certain medications can increase susceptibility.
In addition to these factors, lifestyle choices play a significant role in the development of yeast infections. Wearing tight-fitting clothing or synthetic fabrics can create a warm, damp environment conducive to yeast proliferation. Furthermore, a diet high in sugar can feed the yeast, exacerbating the issue. Understanding these causes is crucial for prevention and effective treatment. Below is a simple table highlighting some common triggers:
| Trigger | Description |
|---|---|
| Antibiotics | Can kill beneficial bacteria, allowing yeast to flourish. |
| Diabetes | High sugar levels can promote yeast growth. |
| Panty Liners | Can trap moisture and heat, creating a breeding ground. |
Types of Yeast Infection Medicines Available
When dealing with a yeast infection, various medications can help alleviate symptoms and eliminate the underlying cause. Over-the-counter options often come in the form of topical treatments or oral medications. Topical treatments include creams, ointments, or suppositories, which can be directly applied to the affected area. These products usually contain agents like clotrimazole, miconazole, or tioconazole. In addition, oral medications, such as fluconazole, are often prescribed for more severe or recurrent cases, providing a convenient one-dose treatment option that targets the infection from within.
For those seeking natural remedies, some prefer to explore homeopathic treatments or probiotics, which may help restore the balance of good bacteria in the body. It’s essential to note that while these alternatives can be advantageous, consulting a healthcare professional is advisable before starting any new treatment. Below is a comparison of common yeast infection medicines:
| Medicine Type | Form | Common Ingredients | Usage |
|---|---|---|---|
| Topical Creams | Ointment/Cream | Clotrimazole, Miconazole | Apply as directed for 3-7 days |
| Oral Medications | Pill | Fluconazole | Single dose, as prescribed |
| Natural Remedies | Capsules/Probiotic | Lactobacillus strains | Daily as a supplement |
Assessing the Effectiveness of Over-the-Counter Treatments
When evaluating the success of over-the-counter treatments for yeast infections, it’s essential to consider several factors that can influence their effectiveness. Many of these products contain active ingredients designed to combat the common culprit, Candida. Users often report varying levels of relief depending on factors such as the severity of the infection, the timing of treatment, and individual health conditions. Here are some key aspects to keep in mind:
- Type of active ingredient: Common options include clotrimazole, miconazole, and tioconazole, each targeting the infection differently.
- Duration of symptoms: Treatment may be more effective if started early in the infection process.
- User adherence: Following the instructions for application can significantly impact the outcome.
In addition, a comparison of different over-the-counter products can shed light on their relative effectiveness. The following table summarizes some popular antifungal agents and their typical application durations:
| Product Name | Active Ingredient | Application Duration |
|---|---|---|
| Monistat 1 | Miconazole | 1 day |
| Lotrimin | Clotrimazole | 3 days |
| Canesten | Clotrimazole | 6 days |
Ultimately, while many over-the-counter treatments can provide effective relief, individuals should monitor their symptoms and consult a healthcare professional if necessary. This approach ensures that any underlying issues are addressed and helps in making informed decisions regarding treatment options.
Prescription Options: When to Consult a Healthcare Provider
When dealing with a yeast infection, it is crucial to identify the right moment to seek advice from a healthcare provider. Symptoms such as severe itching, unusual discharge, or persistent irritation may indicate a more complicated issue that over-the-counter medications cannot address. Additionally, if you’ve experienced multiple yeast infections within a short span, it might be time to consult a professional. This consultation can lead to a tailored treatment plan that considers your medical history and individual needs.
Consider scheduling an appointment with your healthcare provider in the following scenarios:
- Symptoms persist despite treatment
- First-time experience of symptoms
- Recurring infections (four or more in a year)
- Pregnancy or other underlying health conditions
In these cases, your provider may suggest prescription medication, which can be more effective in managing persistent infections. Here’s a quick overview of common prescription options available:
| Medication | Form | Usage |
|---|---|---|
| Fluconazole | Oral Tablet | Single dose or multiple doses over weeks |
| Clotrimazole | Vaginal Cream | Used for up to 7 days |
| Terconazole | Vaginal Suppository | Applied nightly for 3-7 days |
Preventive Measures to Reduce Recurrence
To effectively minimize the chances of a yeast infection returning, it’s essential to incorporate a few lifestyle adjustments and health practices into your routine. Start by ensuring proper hygiene and moisture management in the genital area. This can be achieved through:
- Wearing breathable cotton underwear: This allows for adequate airflow and helps keep the area dry.
- Avoiding douching: Douching can disturb the natural flora, leading to an imbalance.
- Regularly changing out of wet clothes: Whether it’s swimsuits or workout gear, moisture can promote yeast growth.
Nutrition also plays a pivotal role in maintaining a healthy balance of bacteria and yeast in the body. Consider implementing dietary changes that support your immune system and gut health, such as:
- Incorporating probiotics: Foods like yogurt and kefir can help restore natural flora.
- Reducing sugar intake: High sugar levels can fuel yeast growth.
- Staying hydrated: Adequate water intake is crucial for overall health and helps flush out toxins.
Natural Remedies: Exploring Alternative Solutions
For those seeking alternatives to conventional treatments for yeast infections, various natural remedies have gained popularity. These options may offer relief for some individuals, keeping in mind that results can vary. Here are a few commonly explored solutions:
- Probiotics: These beneficial bacteria can help restore the natural balance of flora in the body, potentially preventing the overgrowth of yeast.
- Garlic: Known for its antifungal properties, garlic can be consumed raw or used in cooking to help combat yeast infections.
- Coconut Oil: With its natural antifungal effects, applying coconut oil topically may help soothe irritation and reduce yeast growth.
- Apple Cider Vinegar: Often diluted in water, it is believed to create an unfavorable environment for yeast.
In addition to these remedies, maintaining a healthy lifestyle can play a crucial role in preventing yeast infections. Here’s a quick overview of supportive practices:
| Practice | Benefits |
|---|---|
| Balanced Diet | Supports immune function and reduces sugar intake. |
| Hydration | Flushes out toxins and supports overall body function. |
| Regular Exercise | Boosts immunity and promotes hormonal balance. |
Q&A
Q&A: Understanding Yeast Infection Medicine
Q1: What exactly is a yeast infection?
A1: A yeast infection, also known as candidiasis, is an overgrowth of Candida fungi, particularly Candida albicans, in the body. It commonly occurs in warm, moist areas, such as the vagina, mouth, or skin folds. Symptoms may include itching, irritation, and unusual discharge, which can be uncomfortable but are often manageable with appropriate treatment.
Q2: What types of medicine are available for treating yeast infections?
A2: Yeast infections can be treated with antifungal medications. These come in various forms, including over-the-counter (OTC) options like creams, ointments, or suppositories, as well as prescription medications, such as fluconazole, which is taken orally. The choice of treatment often depends on the severity of the infection and individual preferences.
Q3: How do over-the-counter treatments differ from prescription medications?
A3: Over-the-counter treatments are typically designed for mild to moderate yeast infections and are readily accessible without a prescription. They often include a range of topical agents that can provide quick relief. Prescription medications, on the other hand, are usually recommended for more severe cases or recurrent infections and may offer a broader spectrum of antifungal activity.
Q4: Are there any side effects associated with yeast infection medicines?
A4: Like any medication, yeast infection treatments can have side effects. Common side effects of topical treatments may include burning, itching, or irritation at the application site. Oral antifungal medications, such as fluconazole, may cause nausea, headaches, or abdominal discomfort. It’s essential to discuss potential side effects with a healthcare provider before starting treatment.
Q5: How can I prevent future yeast infections?
A5: Prevention strategies include maintaining good hygiene, wearing breathable cotton underwear, avoiding overly tight clothing, and steering clear of excessive moisture. A balanced diet low in refined sugars can also help, as sugar can promote Candida growth. Additionally, some women find it beneficial to take probiotics to help maintain a healthy balance of bacteria and yeast.
Q6: When should I see a doctor about a yeast infection?
A6: If you experience frequent yeast infections (more than four times a year), if your symptoms persist despite treatment, or if you are unsure whether it’s a yeast infection, it’s wise to consult a healthcare professional. They can provide a proper diagnosis and recommend appropriate treatment options.
Q7: Can yeast infections occur in men?
A7: Yes, yeast infections can affect men, although they are less common. Men can experience symptoms like itching and irritation on the penis or in the groin area. Treatment typically involves antifungal creams or medications, similar to those used for women.
Q8: Is it safe to use yeast infection medicine during pregnancy?
A8: Some antifungal medications are considered safe during pregnancy, while others may not be. It’s crucial for pregnant individuals to consult their healthcare provider before using any medication to ensure both safety for the mother and the developing fetus.
Q9: Can lifestyle choices impact the likelihood of developing a yeast infection?
A9: Absolutely! Lifestyle factors such as diet, hygiene practices, and the use of antibiotics can all influence the risk of developing a yeast infection. A healthy lifestyle that includes a balanced diet, regular exercise, and good hygiene can help reduce the likelihood.
Q10: What should I do if a yeast infection doesn’t improve with treatment?
A10: If symptoms do not improve after completing the recommended course of treatment, or if they worsen, it’s important to follow up with a healthcare provider. There may be an underlying condition or misdiagnosis, requiring further evaluation and tailored treatment.
Understanding yeast infection medicine is vital for effective treatment and prevention. Remember, knowledge is power, and consulting a healthcare professional can illuminate the best path forward for your health.
Concluding Remarks
navigating the world of yeast infection medicine can often feel daunting, but informed choices can lead to effective relief and a return to comfort. From over-the-counter solutions to prescription treatments, there are various options available to suit individual needs. It’s essential to recognize the signs, consult healthcare professionals, and understand the importance of maintaining balance in our bodies. By empowering ourselves with knowledge and taking proactive steps, we can reclaim our health and well-being. Remember, you are not alone in this journey—support and resources are just a step away. Embrace the path to recovery, and let wellness be your guide.
