Title: Navigating the Antibiotic Maze: Understanding Their Role in Sinus Infections
In the intricate landscape of human health, few topics spark as much debate as the use of antibiotics. These powerful medications, designed to combat bacterial infections, have become both a beacon of hope and a source of confusion for many. Among the common ailments that often lead to a visit to the doctor’s office are sinus infections, or sinusitis, which can cause a range of uncomfortable symptoms from persistent nasal congestion to facial pain. But as patients seek relief, the question remains: are antibiotics the answer? This article delves into the role of antibiotics in treating sinus infections, exploring when they are truly necessary, the implications of overuse, and the evolving landscape of treatment options. Join us as we unravel the complexities of this common yet often misunderstood condition, guiding you through the tangled web of medical advice and evidence-based practices.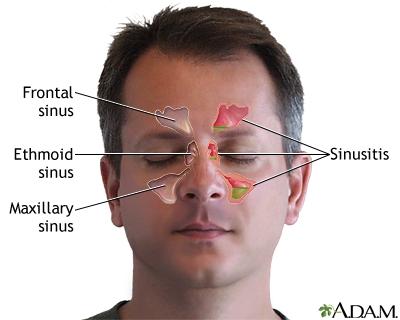
Understanding Sinus Infections and the Role of Antibiotics
Sinus infections, or sinusitis, can be both uncomfortable and disruptive, often stemming from viral infections, allergies, or irritants in the environment. While the body is generally adept at fighting off these invaders, sometimes the sinuses can become inflamed and filled with fluid, leading to bacterial growth. This is where the confusion around the use of antibiotics comes into play. Since most sinus infections are viral, antibiotics are not effective against them. However, if a bacterial infection is suspected, particularly if symptoms persist for longer than 10 days or worsen after initial improvement, antibiotics may be prescribed to help clear the infection.
When considering treatment for sinus infections, it’s essential to understand the role of antibiotics in managing symptoms and promoting recovery. Here’s a brief overview of what you might encounter:
| Type of Infection | Typical Duration | Antibiotic Use |
|---|---|---|
| Viral Sinusitis | 7-10 days | No antibiotics needed |
| Bacterial Sinusitis | 10 days or longer | Possible antibiotic prescription |
| Recurrent Sinusitis | Varies | Referral to specialist may be needed |
By understanding the underlying causes and appropriate treatments for sinus infections, patients can make informed decisions about their health. Consulting with a healthcare professional can determine whether antibiotics are necessary and help explore other therapies to alleviate discomfort and promote healing.
When Are Antibiotics Necessary for Sinus Infections
Determining the need for antibiotics in cases of sinus infections can be tricky. Many sinus infections, particularly those caused by viruses, do not respond to antibiotic treatment. It’s essential to recognize the symptoms that could indicate a bacterial infection rather than a viral one. Some of the key signs include:
- Persistent symptoms lasting more than 10 days
- Severe facial pain or pressure
- Fever above 102°F (39°C) lasting several days
- Thick, green or yellow nasal discharge
If your symptoms align with these criteria, it may be time to consult a healthcare professional for further evaluation. In some cases, a waiting period is advised to see if symptoms improve on their own. If a bacterial infection is confirmed, antibiotics can be an effective treatment option. Here’s a simplified comparison of the common types of sinus infections:
| Type of Sinus Infection | Typical Duration | Antibiotic Need |
|---|---|---|
| Acute Viral Sinusitis | Less than 10 days | No |
| Acute Bacterial Sinusitis | More than 10 days | Yes |
| Chronic Sinusitis | 12 weeks or longer | Consult Required |
Choosing the Right Antibiotic: A Guide for Patients
When it comes to treating a sinus infection, the choice of antibiotic can greatly influence recovery. Not all sinus infections are caused by bacteria; many are viral in nature and won’t respond to antibiotics. Therefore, it’s crucial to consult a healthcare professional who can accurately diagnose the type of infection. If a bacterial infection is confirmed, your doctor may consider several factors before prescribing the appropriate antibiotic. These factors include your medical history, any previous antibiotic use, and potential allergies. Here are some commonly prescribed antibiotics for bacterial sinus infections:
- Amoxicillin – Often the first choice due to its effectiveness against common bacteria.
- Augmentin – A combination of amoxicillin and clavulanate, useful for resistant strains.
- Doxycycline – An alternative for patients allergic to penicillin.
- Cefdinir – A cephalosporin antibiotic for those with specific needs.
Understanding the potential side effects and interactions of these antibiotics is essential. Common side effects can include gastrointestinal discomfort, allergic reactions, and interactions with other medications. To help you navigate your treatment, here’s a quick reference table highlighting some critical information:
| Antibiotic | Common Side Effects | Notes |
|---|---|---|
| Amoxicillin | Diarrhea, rash | First-line treatment for uncomplicated infections. |
| Augmentin | Nausea, diarrhea | Effective against resistant bacteria. |
| Doxycycline | Photosensitivity, upset stomach | Take with food to minimize stomach upset. |
| Cefdinir | Diarrhea, headache | Good alternative for penicillin-allergic patients. |
Potential Side Effects and Risks of Antibiotic Treatment
While antibiotics can be an effective treatment for sinus infections, they are not without their potential side effects and risks. Some individuals may experience mild to moderate reactions, including:
- Dizziness – A common side effect that can interfere with daily activities.
- Gastrointestinal issues – Such as nausea, diarrhea, or abdominal pain, which can disrupt your routine.
- Allergic reactions – Ranging from mild skin rashes to severe anaphylaxis in rare cases.
Moreover, the overuse or misuse of antibiotics can lead to more significant health concerns, including:
- Antibiotic resistance – A growing issue where bacteria evolve to withstand treatment, making infections harder to cure.
- Impact on gut health – Disruption of natural flora can lead to conditions like C. difficile infection.
- Interactions with other medications – It’s vital to inform your healthcare provider about all medications you are taking to avoid adverse effects.
| Potential Risks | Details |
|---|---|
| Side Effects | Nausea, dizziness, skin rashes |
| Resistance | Decreased effectiveness of antibiotics |
| Gut Flora Disruption | Can lead to gastrointestinal infections |
Alternative Treatments for Sinus Infections Beyond Antibiotics
While antibiotics are commonly prescribed for bacterial sinus infections, they are not always necessary or effective, especially in cases caused by viruses. Many individuals are turning to alternative treatments that focus on alleviating symptoms and promoting healing without the use of pharmaceuticals. These methods can provide relief and support the body’s natural defenses. Consider incorporating the following options into your routine:
- Steam Inhalation: Inhaling steam from hot water can help to thin mucus, reduce congestion, and soothe irritated sinus passages.
- Saline Nasal Irrigation: Using a saline solution in a neti pot or squeeze bottle can effectively flush out mucus and allergens.
- Essential Oils: Oils like eucalyptus or peppermint can be used in diffusers or diluted and applied topically to provide relief from sinus pressure.
- Warm Compresses: Applying a warm compress over the sinus areas can help to ease pain and promote drainage.
Moreover, dietary changes and supplements can play a significant role in combating sinus infections. A focus on anti-inflammatory foods can bolster your immune system and facilitate recovery. Here’s a quick reference table to consider:
| Food | Benefit |
|---|---|
| Turmeric | Contains curcumin, known for its anti-inflammatory properties |
| Garlic | Has natural antibacterial and antiviral effects |
| Ginger | Reduces inflammation and can help with mucus clearance |
| Leafy Greens | Rich in vitamins and minerals that support immune function |
Preventive Measures to Reduce Sinus Infections and Antibiotic Dependence
Maintaining optimal sinus health is crucial for preventing infections and reducing reliance on antibiotics. A few lifestyle changes can go a long way in keeping your sinuses clear and healthy. Consider incorporating the following preventive measures into your daily routine:
- Stay Hydrated: Drinking plenty of fluids helps thin mucus, making it easier for your body to drain.
- Humidify Your Environment: Using a humidifier can add moisture to the air, soothing dry nasal passages.
- Practice Good Hygiene: Regular hand washing can prevent the spread of viruses and bacteria that lead to sinus infections.
- Avoid Allergens: Identify and minimize exposure to allergens that can irritate your sinuses, such as pollen and dust.
Additionally, integrating certain foods and practices into your diet may bolster your immune system, making you less susceptible to infections:
| Food | Benefit |
|---|---|
| Garlic | Contains allicin, known for its antimicrobial properties. |
| Citrus Fruits | Rich in Vitamin C, which boosts the immune system. |
| Ginger | Helps reduce inflammation and mucus buildup. |
By adopting these preventive strategies, you can significantly reduce the frequency of sinus infections and the need for antibiotics, promoting a healthier lifestyle overall.
Q&A
Q&A: Understanding Antibiotics for Sinus Infections
Q1: What is a sinus infection, and how does it occur?
A: A sinus infection, or sinusitis, occurs when the nasal cavities become swollen or inflamed, often due to bacteria, viruses, or allergens. This blockage can trap mucus, leading to pressure, pain, and the characteristic symptoms of sinusitis, including nasal congestion, facial swelling, and headaches.
Q2: When should someone consider using antibiotics for a sinus infection?
A: Antibiotics are typically reserved for cases of acute bacterial sinusitis, which usually lasts less than four weeks. If symptoms persist for more than ten days, worsen after initial improvement, or are accompanied by a high fever, it may be time to consult a healthcare professional about the potential need for antibiotics.
Q3: Are all sinus infections treated with antibiotics?
A: Not at all! In fact, most sinus infections are viral in nature. Antibiotics are ineffective against viruses, so they are only prescribed if a bacterial infection is confirmed or highly suspected. It’s crucial to avoid unnecessary antibiotic use to prevent antibiotic resistance.
Q4: What are the common antibiotics prescribed for sinus infections?
A: Commonly prescribed antibiotics for bacterial sinus infections include amoxicillin, amoxicillin-clavulanate (Augmentin), and, in some cases, doxycycline. The choice depends on the patient’s medical history and local bacterial resistance patterns.
Q5: What are the potential side effects of taking antibiotics for sinus infections?
A: Side effects can range from mild to moderate and might include gastrointestinal issues such as nausea, diarrhea, and stomach upset. More serious effects, though rare, can include allergic reactions. It’s always best to discuss potential side effects with a healthcare provider before starting any medication.
Q6: How can one alleviate sinus infection symptoms without antibiotics?
A: Many people find relief through home remedies such as saline nasal sprays, steam inhalation, staying hydrated, and using over-the-counter pain relievers like ibuprofen or acetaminophen. Rest and a humid environment can also help soothe irritated sinuses.
Q7: What should a patient do if their symptoms do not improve after taking antibiotics?
A: If symptoms persist or worsen despite antibiotic treatment, it’s essential to follow up with a healthcare professional. They may reassess the condition, considering factors such as the possibility of a different type of infection, chronic sinusitis, or other underlying issues.
Q8: Can lifestyle changes help prevent sinus infections?
A: Absolutely! Maintaining good nasal hygiene, avoiding allergens or irritants, staying hydrated, and managing allergies can significantly reduce the risk of developing sinus infections. Regular exercise and a balanced diet also contribute to overall immune health.
Q9: Is it safe to self-diagnose a sinus infection and seek antibiotics?
A: Self-diagnosis can be misleading and potentially harmful. It’s always advisable to seek a healthcare professional’s insight. They can provide an accurate diagnosis and appropriate treatment plan, which may or may not include antibiotics.
Q10: What’s the bottom line on antibiotics for sinus infections?
A: While antibiotics can be an effective treatment for bacterial sinus infections, they are not always necessary. Understanding the nature of the infection and consulting with a healthcare provider are key steps in ensuring effective and safe treatment. Always prioritize health and informed decision-making over self-medication.
In Summary
while antibiotics can play a crucial role in treating certain types of sinus infections, it’s essential to approach their use with a discerning eye. Understanding the underlying cause of your symptoms—be it viral, bacterial, or allergic—can significantly influence the effectiveness of treatment. As we’ve explored, the overuse of antibiotics poses risks not only to individual health but also to public health at large, making responsible usage paramount. Consulting with a healthcare provider remains the best course of action to ensure the right diagnosis and treatment plan. By being informed and proactive in our healthcare choices, we can navigate the complexities of sinus infections and antibiotics with greater confidence, paving the way for a healthier tomorrow.
