In the intricate tapestry of global health, few threads are as vibrant and elusive as the influenza virus. Each year, as the seasons change and the air turns crisp, communities brace themselves for the arrival of this microscopic foe, a shape-shifting agent that has danced through human history for centuries. With its ability to mutate and adapt, the influenza virus presents a perennial challenge for scientists and public health officials, sparking a relentless pursuit of understanding and prevention. As we delve into the world of this formidable virus, we uncover not only its biological complexities but also its far-reaching impact on society, underscoring the vital importance of vigilance and research in our ongoing battle against this seasonal adversary. Join us as we explore the science, history, and implications of influenza, illuminating the nuances of a virus that continues to influence our lives in profound ways.
Understanding the Influenza Virus: Mechanisms and Variants
The influenza virus is a complex pathogen with a remarkable ability to adapt and evolve, which poses significant challenges to public health. It primarily exists in three types: A, B, and C, with type A being the most prevalent and known for its severe outbreaks. The virus’s structure features an outer lipid envelope containing hemagglutinin (HA) and neuraminidase (NA) proteins that play crucial roles in its lifecycle. These proteins are responsible for the virus’s ability to enter host cells and for the release of new viral particles, respectively. The genetic material of the virus, composed of eight segments of RNA, allows for a high rate of mutation and genetic reassortment, leading to the emergence of new strains that can evade the immune response.
Understanding the variants of the influenza virus is essential for effective prevention and treatment strategies. Notably, the subtypes of the influenza A virus are categorized based on the combinations of HA and NA proteins, such as H1N1 and H3N2. Each year, health organizations monitor these variants to update the flu vaccine, making it a moving target. Here’s a concise overview of some key influenza variants and their implications:
| Variant | Transmission | Severity |
|---|---|---|
| H1N1 | Human and Swine | Moderate |
| H3N2 | Human | Severe |
| B Victoria | Human | Mild |
| B Yamagata | Human | Mild |
As we continue to study these mechanisms and variants, it becomes clear that comprehensive surveillance and research are vital in combating seasonal flu and preventing potential pandemics. Enhanced understanding of viral dynamics will also aid in developing better vaccines and antiviral treatments, ensuring that we stay one step ahead in the ongoing battle against influenza.
The Impact of Seasonal Influenza: Symptoms and Transmission Dynamics
Seasonal influenza presents a range of common symptoms that can significantly impact individuals and communities each year. The most frequently reported symptoms include:
- Fever or chills
- Cough
- Sore throat
- Runny or stuffy nose
- Muscle or body aches
- Headaches
- Fatigue
- Some may experience vomiting or diarrhea (more common in children)
In terms of transmission dynamics, the influenza virus spreads primarily through respiratory droplets when an infected person talks, coughs, or sneezes. Additionally, the virus can survive on surfaces for hours, leading to indirect transmission through contact with contaminated objects. Key factors influencing the spread include:
- Population density
- Seasonal changes, particularly during colder months
- Vaccination rates within communities
- Hygiene practices such as handwashing and use of masks
Understanding these dynamics is crucial for health professionals and policymakers in implementing effective public health strategies. The table below summarizes the peak influenza season periods across different regions:
| Region | Peak Season Months |
|---|---|
| North America | November to March |
| Europe | December to February |
| Australia | June to August |
| Asia | Variable, often winter months |
Vaccination Strategies: Best Practices for Protection Against Influenza
To effectively combat the influenza virus, implementing a comprehensive vaccination strategy is essential. Annual vaccination remains the cornerstone of influenza prevention, as the virus frequently mutates and new strains emerge each season. It’s crucial to tailor vaccination campaigns to target high-risk populations, including the elderly, children, and individuals with chronic health conditions. Consider the following best practices:
- Education and Awareness: Inform communities about the benefits of vaccination.
- Accessibility: Provide vaccines in various locations, including schools and workplaces.
- Incentives: Encourage vaccination through incentives like free flu shots or health insurance discounts.
- Collaboration: Partner with local healthcare providers to enhance outreach and delivery.
Monitoring vaccine efficacy and adjusting strategies based on emerging data is equally important. Seasonal flu vaccines differ in formulation, so it’s vital to keep the public informed about the most effective options each year. Establishing a feedback loop can help refine these strategies over time. Consider setting up a tracking system that includes:
| Vaccination Method | Effectiveness | Target Group |
|---|---|---|
| Inactivated Virus Vaccine | Varies (40-60%) | General Public |
| Live Attenuated Vaccine | Higher in some populations | Healthy Children |
| Recombinant Vaccine | Potentially higher | High-Risk Individuals |
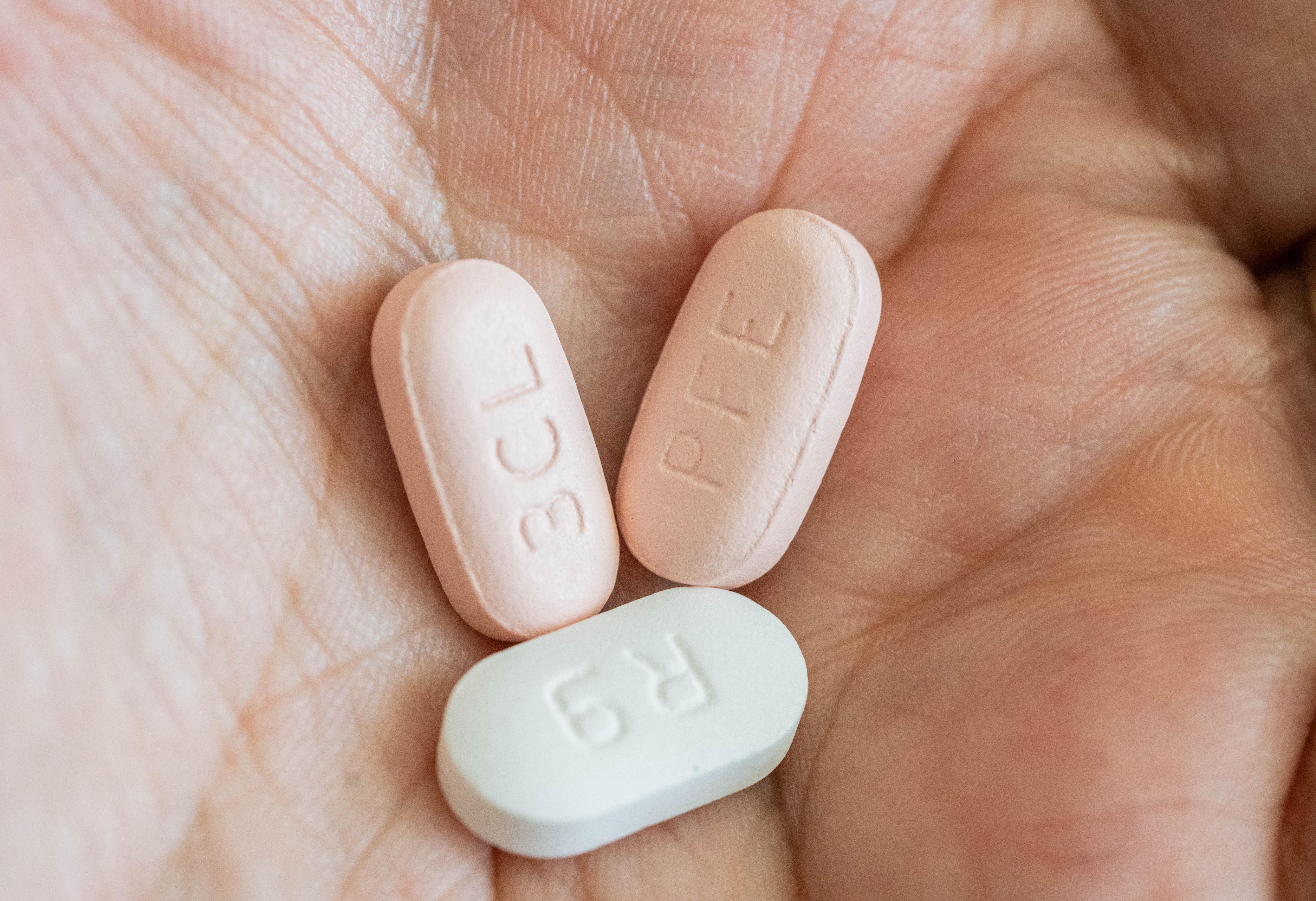
Antiviral Treatments: Options for Effective Management of Influenza
Antiviral medications play a critical role in the effective management of influenza, particularly for those at high risk of complications. Oseltamivir (commonly known as Tamiflu) and Zanamivir (Relenza) are two prominent options that can help reduce the severity and duration of symptoms when administered within the first 48 hours of illness onset. These treatments target the influenza virus’s ability to replicate, thereby aiding the body’s immune response. Moreover, Peramivir, an intravenous antiviral, is particularly useful for patients unable to take oral medications, enhancing treatment accessibility for various populations.
In addition to these established antiviral options, emerging therapies and novel compounds are continuously being researched to bolster our arsenal against influenza. Baloxavir marboxil (Xofluza) is a new single-dose oral antiviral that shows promise in treating uncomplicated influenza. Furthermore, the development of vaccines remains a cornerstone in preventing influenza outbreaks. Here’s a brief comparison of the most common antiviral treatments:
| Antiviral | Type | Administration | Duration of Treatment |
|---|---|---|---|
| Oseltamivir | Neuraminidase Inhibitor | Oral | 5 days |
| Zanamivir | Neuraminidase Inhibitor | Inhalation | 5 days |
| Peramivir | Neuraminidase Inhibitor | Intravenous | 1 dose |
| Baloxavir marboxil | Endonuclease Inhibitor | Oral | 1 dose |
Preventive Measures: Lifestyle Changes to Reduce Infection Risk
Adopting a healthier lifestyle can significantly decrease your risk of contracting the influenza virus. Start by focusing on a balanced diet rich in fruits, vegetables, and whole grains. These foods are packed with essential nutrients that bolster your immune system. Additionally, incorporate lean proteins and healthy fats to support overall health. Staying hydrated is equally important; strive to drink at least eight glasses of water a day. Limit your intake of processed foods and sugars, which can weaken your immune response, making your body more susceptible to infections.
Physical activity is another crucial component in reducing your infection risk. Aim for a minimum of 150 minutes of moderate aerobic exercise each week. This can include activities such as brisk walking, cycling, or swimming. Furthermore, prioritize good sleep hygiene—aim for 7-9 hours of quality sleep each night to allow your body to recover and repair. Stress management techniques, such as meditation, yoga, or deep-breathing exercises, can also play a vital role in maintaining a robust immune system. Remember, consistency is key, so make these lifestyle changes a regular part of your routine.
Public Health Response: Strategies for Containing Influenza Outbreaks
Effective public health responses to influenza outbreaks rely on a multifaceted approach that emphasizes prevention, early detection, and rapid intervention. Vaccination remains the cornerstone of these strategies, ensuring that vulnerable populations, including the elderly and those with underlying health conditions, receive their annual flu shots. In addition to vaccinations, public health officials advocate for community awareness campaigns that educate the public about hygiene practices, such as frequent handwashing and respiratory etiquette. The use of social media platforms can enhance outreach, allowing for real-time updates and information dissemination regarding outbreak status and prevention tips.
Another critical component of managing influenza outbreaks involves surveillance and data collection. By implementing robust surveillance systems, health authorities can closely monitor flu activity, detect anomalies in infection rates, and respond swiftly. This data can be visualized through timely reports and interactive dashboards that engage both the public and healthcare professionals. Collaboration with healthcare providers is essential, as they play a vital role in identifying cases and reporting them to health departments. Moreover, the establishment of regional flu response teams can facilitate coordinated efforts across jurisdictions, ensuring a comprehensive approach to mitigate the impact of influenza on communities.
Q&A
Q&A: Understanding the Influenza Virus
Q1: What exactly is the influenza virus?
A1: The influenza virus is a contagious virus that primarily affects the respiratory system. It belongs to the Orthomyxoviridae family and is known for its ability to mutate and evolve rapidly, leading to seasonal outbreaks and occasional pandemics. There are four main types of influenza viruses: A, B, C, and D, with types A and B being responsible for the majority of seasonal flu cases in humans.
Q2: How does the influenza virus spread?
A2: The influenza virus spreads primarily through respiratory droplets when an infected person coughs, sneezes, or talks. It can also be contracted by touching surfaces contaminated with the virus and then touching one’s face—particularly the mouth, nose, or eyes. This makes it highly transmissible, especially in crowded or enclosed environments.
Q3: What are the symptoms of an influenza infection?
A3: Symptoms of influenza typically include sudden onset of fever, chills, cough, sore throat, runny or stuffy nose, muscle or body aches, headaches, and fatigue. Some individuals may also experience gastrointestinal symptoms, such as nausea or diarrhea, although these are more common in children than adults.
Q4: How can one differentiate between influenza and a common cold?
A4: While both influenza and the common cold are respiratory illnesses, they are caused by different viruses and exhibit different severity levels. Influenza usually comes on suddenly and is characterized by high fever and significant body aches, while colds tend to develop gradually and are generally milder, often involving more nasal congestion and sneezing than severe systemic symptoms.
Q5: Are there effective treatments for influenza?
A5: Yes, antiviral medications such as oseltamivir (Tamiflu) and zanamivir (Relenza) can help shorten the duration of the illness and reduce severity if taken within the first 48 hours of symptom onset. Additionally, supportive care like hydration, rest, and over-the-counter medications for pain and fever can aid recovery.
Q6: What preventive measures can be taken to avoid catching the flu?
A6: The most effective way to prevent influenza is through vaccination. Annual flu shots are recommended for most individuals, especially vulnerable populations such as the elderly, young children, and those with chronic health conditions. Other preventive measures include frequent handwashing, avoiding close contact with sick individuals, and maintaining good respiratory hygiene, such as covering one’s mouth when coughing or sneezing.
Q7: Why is it important to monitor influenza outbreaks?
A7: Monitoring influenza outbreaks is crucial for public health as it helps identify trends in virus circulation, assess vaccine effectiveness, and implement timely interventions to mitigate the spread. Understanding these patterns can also assist in predicting potential pandemics and preparing healthcare systems accordingly.
Q8: Are there any misconceptions about the influenza virus that should be addressed?
A8: Yes, several common misconceptions exist. One prevalent myth is that the flu vaccine can cause the flu; however, the vaccine contains inactivated virus particles or weakened strains and cannot cause illness. Another misconception is that the flu is just a “bad cold.” In reality, influenza can lead to severe complications, such as pneumonia and hospitalization, especially in at-risk populations.
Q9: What role does climate play in influenza transmission?
A9: Climate can influence the seasonality of influenza. The virus tends to thrive in colder, drier conditions, which is why flu cases typically rise in the fall and winter months in temperate regions. However, this is not the only factor; human behavior, population density, and public health interventions also play significant roles in influenza dynamics.
Q10: What does the future hold for influenza virus research and prevention?
A10: The future of influenza research focuses on improving vaccine effectiveness, developing universal flu vaccines that offer broader protection, and enhancing surveillance systems to monitor virus mutations. Advances in genetic sequencing and bioinformatics are aiding researchers in understanding the influenza virus better and preparing for potential outbreaks, making public health responses more efficient and effective.
In Retrospect
As we draw the curtain on our exploration of the influenza virus, we are reminded of the delicate balance between nature and human health. This microscopic adversary, with its ever-evolving arsenal, continues to challenge our understanding and resilience. From the historical pandemics that have shaped public health policies to the advancements in vaccines that offer hope for the future, the journey of combating influenza is a testament to human ingenuity and perseverance.
As we navigate through the changing seasons and the annual resurgence of flu activity, it’s crucial to remain informed and vigilant. Just as the virus adapts, so too must our strategies for prevention and treatment. In this interconnected world, the fight against influenza is not just an individual endeavor but a collective one that requires global cooperation and awareness.
With knowledge as our ally, we can better arm ourselves against this age-old foe. So, as you move through this flu season and beyond, remember the lessons learned and the importance of staying engaged in the ongoing conversation about infectious diseases. Together, we can create a healthier future, one flu season at a time.
