Unlocking the Mystery of TB: Understanding Tuberculosis in the Modern World
In the shadows of modern medicine, where advancements have tamed many once-feared ailments, tuberculosis (TB) continues to persist as a formidable foe. Despite its ancient roots, this infectious disease remains one of the leading causes of morbidity and mortality worldwide. As we delve into the intricate tapestry of TB, we unravel not only the biological mechanisms that allow it to thrive but also the social and economic factors that perpetuate its spread. From the bustling streets of urban centers to remote rural communities, TB weaves its way through the fabric of society, challenging health systems and igniting conversations about equity, access, and innovation in healthcare. This article aims to shed light on the complexities of TB, exploring its history, impact, and the ongoing efforts to combat it in an ever-evolving global landscape. Join us as we navigate through the facts, figures, and narratives that define tuberculosis today.
Understanding Tuberculosis: An Overview of Causes and Symptoms
Tuberculosis (TB) is a contagious infection primarily affecting the lungs, but it can also spread to other parts of the body. Understanding the causes of TB is essential for prevention and control. The primary culprit is the bacterium Mycobacterium tuberculosis, which spreads through the air when an infected person coughs or sneezes. Those with weakened immune systems, such as individuals with HIV, malnutrition, or chronic health conditions, are particularly at risk. Other significant factors include overcrowded living conditions, poor ventilation, and inadequate healthcare access, which create environments conducive to the transmission of this disease.
Identifying the symptoms of TB early can significantly improve treatment outcomes. Common symptoms include:
- Persistent cough lasting more than three weeks
- Chest pain or discomfort when breathing or coughing
- Weight loss and loss of appetite
- Fatigue and weakness
- Fever and night sweats
Recognizing these signs is crucial for timely diagnosis and intervention, as untreated TB can lead to serious health complications and increased transmission risks.
The Global Impact of Tuberculosis: Statistics and Trends
Tuberculosis (TB) remains one of the world’s deadliest infectious diseases, with a significant toll on global health. In 2021 alone, approximately 10.6 million people fell ill with TB, and 1.6 million died from the disease, according to the World Health Organization. The burden of TB is not uniformly distributed; it predominantly affects low- and middle-income countries. The following statistics illustrate its widespread impact:
- India, with an estimated 26% of global TB cases.
- China and Indonesia rank second and third, contributing 8% and 6% respectively.
- Sub-Saharan Africa is particularly affected, with high prevalence rates exacerbated by HIV co-infection.
Recent trends indicate a complex battle against TB, as efforts to eliminate the disease face hurdles such as drug resistance and healthcare access. The emergence of multidrug-resistant TB (MDR-TB) has complicated treatment protocols, making it more difficult to achieve successful outcomes. The following table highlights the global prevalence of MDR-TB across various regions:
| Region | Percentage of MDR-TB Cases |
|---|---|
| Eastern Europe | 20% |
| Southeast Asia | 10% |
| Western Pacific | 8% |
Addressing the global impact of TB requires a multifaceted approach, including heightened awareness, improved diagnostics, and equitable access to treatment. As nations grapple with the resurgence of this ancient disease, collaborative efforts are essential in paving the way towards a TB-free future.
Diagnosis and Testing: Navigating the Path to Early Detection
Understanding the importance of timely diagnosis in the fight against tuberculosis (TB) is crucial for effective management and treatment. Early detection plays a vital role in preventing the spread of the infection and reducing the risk of severe health implications. A variety of diagnostic tools are available, each with its unique strengths. These include:
- Skin Tests: The Mantoux tuberculin skin test is a classic method where a small amount of purified protein derivative (PPD) is injected into the skin.
- Blood Tests: Interferon-gamma release assays (IGRAs) provide a specific response related to TB infection.
- Imaging: Chest X-rays and CT scans help visualize the lungs for signs of TB disease.
- Sputum Tests: Analyzing sputum samples can confirm the presence of the TB bacteria.
In addition to these methods, understanding the signs and symptoms associated with TB can lead to quicker medical intervention. Common symptoms include persistent cough, weight loss, fever, and night sweats. If left untreated, TB can lead to significant health complications. Therefore, awareness of these warning signs can foster proactive health-seeking behavior. Below is a concise overview of symptoms and their implications:
| Symptom | Implication |
|---|---|
| Cough lasting more than 3 weeks | Possible lung involvement |
| Unexplained weight loss | Systemic effects of infection |
| Fever | Indicates active infection |
| Night sweats | Common in active TB cases |
Treatment Options for Tuberculosis: A Comprehensive Guide
Tuberculosis (TB) treatment typically involves a multi-drug regimen that is essential to effectively combat the infection and prevent the development of drug-resistant strains. The standard course of treatment usually spans six months, during which patients are administered a combination of antibiotics. Key medications include:
- Isoniazid – targets the bacterial cell wall
- Rifampicin – inhibits RNA synthesis
- Pyrazinamide – works to disrupt the bacteria’s energy production
- Ethambutol - interferes with cell wall synthesis
In cases where drug resistance is present, a more aggressive treatment approach is required. This may involve the use of second-line medications, which can be less effective and have more side effects. These options include:
- Ciprofloxacin - a fluoroquinolone antibiotic
- Amikacin – an injectable aminoglycoside
- Levofloxacin – a broad-spectrum antibiotic
- Linezolid - effective against resistant strains
| Drug Category | Duration | Common Side Effects |
|---|---|---|
| First-line | 6 months | Nausea, liver toxicity |
| Second-line | 9-24 months | More severe: hearing loss, anemia |
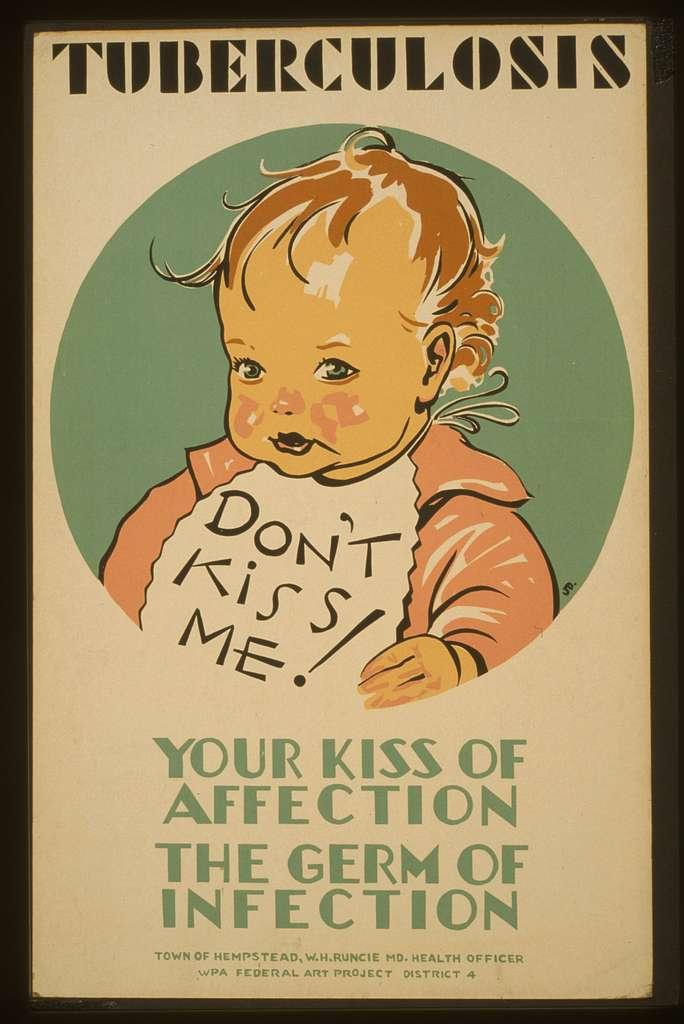
Preventive Measures: Strategies to Reduce Tuberculosis Transmission
To effectively curb the spread of tuberculosis, it’s essential to implement comprehensive preventive measures that engage communities and healthcare systems alike. Education and awareness are key components; informing the public about how TB spreads, its symptoms, and the importance of seeking treatment can significantly diminish its transmission. Programs that focus on high-risk populations, such as those in close living quarters or individuals with weakened immune systems, are particularly vital. Additionally, encouraging the use of protective measures, such as wearing masks in crowded places and ensuring good ventilation in living and working environments, can help reduce exposure.
Another crucial strategy involves screening and vaccination. Regular screening for TB, especially in high-risk groups, allows for early detection and treatment, limiting the potential for further spread. The BCG vaccine, while not universally effective, provides some protection, especially in children. Collaboration between local governments and healthcare providers can facilitate contact tracing efforts, ensuring that those who have been in close contact with an infected individual are tested and treated if necessary. By fostering a community approach that includes these strategies, we can create a robust defense against tuberculosis transmission.
Living with Tuberculosis: Support Systems and Lifestyle Adjustments
Living with tuberculosis (TB) can be challenging, but establishing a solid support system is crucial for managing both the physical and emotional aspects of the illness. Family and friends play a significant role in providing encouragement and practical assistance throughout the treatment journey. Consider joining support groups to connect with others who share similar experiences. These groups can offer a safe space for sharing personal stories, coping strategies, and insights that may help alleviate feelings of isolation. Additionally, engaging with healthcare professionals who specialize in TB can provide personalized advice and resources tailored to your specific situation.
Adapting your lifestyle is essential in promoting recovery and ensuring a better quality of life. Incorporating nutritious foods and staying hydrated can bolster your immune system, aiding your body in fighting off the infection. Regular exercise within your limits is beneficial as well, enhancing your overall well-being. Here’s a simple table illustrating key lifestyle adjustments to consider:
| Adjustment | Description |
|---|---|
| Nutrition | Focus on a balanced diet rich in vitamins and minerals. |
| Hydration | Drink plenty of water to support bodily functions. |
| Rest | Ensure adequate sleep to aid recovery. |
| Exercise | Engage in light physical activity to maintain strength. |
Q&A
Q&A on Tuberculosis (TB)
Q1: What is tuberculosis (TB) and how does it affect the body?
A1: Tuberculosis, often simply referred to as TB, is an infectious disease primarily caused by the bacterium Mycobacterium tuberculosis. It mainly affects the lungs, but can also target other parts of the body such as the kidneys, spine, and brain. The infection usually starts when someone breathes in droplets containing the bacteria, often from an infected person’s cough or sneeze. Once inside, the bacteria can evade the immune system and multiply, leading to symptoms like chronic cough, weight loss, fever, and night sweats.
Q2: How is TB transmitted from one person to another?
A2: TB is transmitted through the air, which makes it highly communicable in close quarters. When an infected person coughs, sneezes, or even speaks, tiny droplets containing the bacteria can be released into the air. If someone else inhales these droplets, they may become infected. However, it’s important to note that not everyone who breathes in the bacteria will develop TB; many may carry the bacteria without showing symptoms, a condition known as latent TB.
Q3: Can TB be prevented?
A3: Yes, TB can be prevented through several measures. Vaccination with the Bacillus Calmette-Guérin (BCG) vaccine is one method, particularly in countries with high rates of TB. Additionally, improving ventilation in living spaces, wearing masks, and practicing good hygiene can help reduce transmission. It’s vital for those diagnosed with TB to follow treatment plans diligently to minimize the risk of spreading the disease to others.
Q4: What are the common symptoms of TB, and when should someone seek medical attention?
A4: Common symptoms of TB include a persistent cough that lasts for three weeks or longer, chest pain, coughing up blood, unintentional weight loss, fatigue, fever, and night sweats. If someone experiences these symptoms—especially if they have been in close contact with someone diagnosed with TB—they should seek medical attention promptly. Early diagnosis and treatment are crucial for both recovery and preventing further transmission.
Q5: How is TB diagnosed?
A5: TB can be diagnosed through a combination of methods. The most common initial test is the tuberculin skin test (TST), where a small amount of TB protein is injected under the skin, and the reaction is measured after 48-72 hours. Another method is the interferon-gamma release assay (IGRA), a blood test that can indicate whether a person has been infected with TB bacteria. If these tests suggest TB infection, further evaluation, such as a chest X-ray and sputum culture, may be conducted to confirm active disease.
Q6: What is the treatment for TB?
A6: Treatment for TB typically involves a lengthy course of antibiotics, usually lasting six to nine months. The most common medications include isoniazid, rifampin, ethambutol, and pyrazinamide. It’s essential to complete the entire course of treatment to fully eradicate the bacteria and prevent drug-resistant strains from developing. Directly Observed Therapy (DOT) is often recommended, where a healthcare provider observes the patient taking their medications to ensure compliance.
Q7: What are the challenges faced in the fight against TB today?
A7: The fight against TB faces several significant challenges. The emergence of drug-resistant TB strains is one of the most pressing issues, making treatment more complicated and less effective. Stigma surrounding the disease can also hinder individuals from seeking help. Additionally, socio-economic factors such as poverty, inadequate healthcare access, and malnutrition contribute to the spread and incidence of TB. Global efforts continue to focus on improving detection, treatment, and education to combat these barriers.
Q8: How does TB impact communities on a larger scale?
A8: TB can have far-reaching effects on communities. High rates of infection can strain healthcare systems, diverting resources from other health issues. The disease can also affect economic productivity, as individuals suffering from TB may be unable to work, leading to loss of income for families and communities. Furthermore, the psychological burden of living with TB and the associated stigma can have lasting effects on mental health and social dynamics. Addressing TB effectively requires a comprehensive approach that includes medical treatment, community awareness, and support systems.
Insights and Conclusions
the multifaceted nature of tuberculosis (TB) urges us to look beyond its clinical implications and delve into the broader societal context surrounding this ancient disease. As we navigate the challenges posed by TB — from its biological complexities to the social stigmas it engenders — it becomes clear that a comprehensive approach is essential. Awareness, education, and global collaboration are key to dismantling the barriers that hinder progress. While the fight against TB may seem daunting, the collective efforts of healthcare professionals, researchers, and communities offer a beacon of hope. Together, we can cultivate a future where TB is not just a chapter in our medical history, but a story of resilience and triumph over adversity. Let us continue to stand united in the pursuit of a world free from the shadows of TB, fostering an environment where health, dignity, and opportunity flourish for all.