Navigating the Culinary Landscape of Crohn’s Disease: A Guide to Dietary Choices
For those living with Crohn’s disease, the journey often involves a delicate dance between managing symptoms and enjoying life’s simplest pleasures—like sharing a meal. This chronic inflammatory bowel condition can be unpredictable, leading many to seek solace in dietary adjustments that not only soothe their digestive systems but also nourish their bodies. But what does a Crohn’s disease diet truly entail? Is it a restrictive regimen or an opportunity to explore new flavors and foods? In this article, we will delve into the intricacies of a Crohn’s-friendly diet, offering insights and practical tips aimed at fostering both health and enjoyment for those navigating the challenges of this condition. Whether you are newly diagnosed or a seasoned traveler on this path, understanding the role of diet is essential for thriving with Crohn’s. Join us as we unravel the complexities of food choices that can empower and support those on this unique culinary journey.
Understanding the Role of Diet in Managing Crohns Disease
Diet plays a pivotal role in managing Crohn’s disease, acting as a powerful tool to alleviate symptoms and promote overall well-being. Patients often find that certain foods can trigger flare-ups, making it essential to identify and avoid these irritants. A tailored diet can help minimize inflammation and optimize nutrient absorption, which is crucial given the malabsorption issues commonly associated with the condition. Individuals with Crohn’s may benefit from a careful selection of digestible foods that are less likely to irritate the gastrointestinal tract. Some of these foods include:
- Lean proteins: Skinless poultry, fish, and eggs
- Low-fiber fruits: Bananas, applesauce, and canned peaches
- Refined grains: White rice, pasta, and bread
Additionally, incorporating anti-inflammatory options can further support gut health. Patients should consider adopting a balanced diet rich in nutrients to counteract deficiencies often seen in Crohn’s sufferers. Keeping a food diary may be beneficial for tracking which foods lead to discomfort and which provide relief. Below is a simple table highlighting beneficial and potentially harmful foods:
| Beneficial Foods | Poorly Tolerated Foods |
|---|---|
| Cooked vegetables | Raw vegetables |
| Oatmeal | Whole grains |
| Yogurt | Dairy products |
Identifying Trigger Foods: A Guide to Personalizing Your Meal Plan
Understanding your body’s unique responses to different foods is crucial in managing Crohn’s disease. Trigger foods can vary greatly from person to person, making it essential to maintain a food diary to track your meals and symptoms. By documenting your meals and how you feel afterward, you can begin to identify patterns that may indicate which foods exacerbate your condition. Look out for common culprits such as:
- Dairy products: Many individuals with Crohn’s disease are lactose intolerant.
- High-fiber foods: Nuts, seeds, and whole grains may cause discomfort during flare-ups.
- Spicy foods: These can irritate the digestive tract.
- Processed foods: High in additives and preservatives that may trigger symptoms.
Once you identify potential trigger foods, you can begin to create a personalized meal plan that prioritizes foods that are gentle on your system. Incorporating foods that promote healing and comfort is key. Consider including the following options in your diet:
| Food Group | Recommended Foods |
|---|---|
| Proteins | Lean meats, fish, eggs |
| Fruits | Bananas, applesauce, canned fruits |
| Vegetables | Cooked carrots, spinach, zucchini |
| Grains | White rice, plain pasta, oatmeal |
By focusing on these gentle options and continuing to refine your meal plan based on your observations, you can take significant steps toward managing your symptoms effectively. Remember that each person’s journey with Crohn’s disease is unique, so patience and persistence are vital in finding the right balance for your dietary needs.
Nutrient-Rich Choices: Building a Balanced Diet for Crohns Patients
Creating a balanced diet for those with Crohn’s disease requires careful consideration to ensure that meals are not only nutritious but also gentle on the digestive system. Incorporating easily digestible foods is essential, as it can help minimize flare-ups and promote overall gut health. Focus on whole grains, such as oatmeal and brown rice, which provide fiber without overwhelming the gastrointestinal tract. Additionally, including lean proteins like chicken, turkey, and fish can support tissue repair and immune function. Don’t forget to add healthy fats, such as avocado and olive oil, to enhance nutrient absorption while providing a soothing effect on the digestive lining.
Moreover, hydration plays a crucial role in managing Crohn’s symptoms. Aim to drink plenty of fluids throughout the day, particularly water and mild herbal teas, to help maintain hydration levels. It’s also beneficial to include a variety of fruits and vegetables, but be mindful of how they are prepared; cooking them can make them easier to digest. Below is a simple guide to some recommended foods:
| Food Category | Examples |
|---|---|
| Whole Grains | Oatmeal, Quinoa, Brown Rice |
| Lean Proteins | Chicken, Turkey, Fish |
| Healthy Fats | Avocado, Olive Oil, Nut Butters |
| Fruits | Bananas, Apples (cooked), Melons |
| Vegetables | Carrots, Spinach (cooked), Zucchini |
The Importance of Hydration: Staying Healthy During Flares
Hydration plays a vital role in managing Crohn’s disease, especially during flare-ups when the body is under increased stress. Maintaining adequate fluid intake helps to support digestion, flush out toxins, and keep the body’s systems running smoothly. When experiencing symptoms such as diarrhea, dehydration becomes a significant risk, potentially exacerbating discomfort and leading to further complications. Therefore, it’s essential for individuals to be proactive about their hydration, opting for fluids that not only replenish lost electrolytes but also provide additional health benefits.
Incorporating a variety of hydrating options into your daily routine can be both enjoyable and beneficial. Consider these sources to enhance your hydration strategy:
- Water: The simplest and most effective choice.
- Herbal teas: Naturally caffeine-free and soothing.
- Broths: Nutrient-rich and comforting during flare-ups.
- Electrolyte drinks: Help to maintain balance and replenish lost minerals.
- Fresh fruits and vegetables: Watermelon, cucumbers, and oranges can provide hydration and essential nutrients.
| Food Item | Hydration Level (%) |
|---|---|
| Watermelon | 92% |
| Cucumber | 95% |
| Strawberries | 91% |
| Broth | 95% |
Staying hydrated is an essential component of managing Crohn’s disease, especially during challenging times. By being mindful of your fluid intake and choosing hydrating options that suit your taste, you can support your body’s resilience, ultimately enhancing your quality of life. Remember, listening to your body’s needs and adjusting your hydration strategy accordingly can make a significant difference in your overall well-being.
Mindful Eating: Strategies to Enhance Digestion and Comfort
Embracing mindful eating can significantly improve the digestive experience for those managing Crohn’s disease. Start by creating a peaceful eating environment. Minimize distractions and focus solely on your meal. This allows your body to signal hunger and fullness cues more effectively, helping you make healthier choices. Consider using smaller plates to control portion sizes and prevent overeating, which can exacerbate symptoms. Furthermore, chew your food thoroughly and savor each bite—this simple practice aids in digestion by breaking food down before it enters the stomach.
Additionally, keeping a food diary can illuminate how various foods affect your body. By noting down what you eat and your subsequent feelings or symptoms, you can identify triggers that may worsen your condition. Implement strategies such as eating smaller, more frequent meals instead of three large ones. This not only eases the digestive burden but also maintains energy levels throughout the day. Below is a simple table to help you track your meals and symptoms:
| Date | Meal | Symptoms |
|---|---|---|
| MM/DD | Breakfast | None |
| MM/DD | Lunch | Mild Cramping |
| MM/DD | Dinner | None |
Exploring Supplements: When Diet Isnt Enough for Nutritional Needs
Individuals managing Crohn’s disease often face unique challenges when it comes to nutrition. While a well-balanced diet is essential, sometimes it simply isn’t enough to meet the body’s needs. This is where supplements can play a crucial role, helping to bridge the nutritional gaps that may arise from dietary restrictions or malabsorption issues. Certain vitamins and minerals, such as Vitamin D, B12, and Iron, are frequently deficient in those with Crohn’s, making supplementation a viable option to support overall health.
When considering supplements, it’s essential to select high-quality products tailored to individual needs. Consulting with a healthcare professional can provide personalized recommendations based on specific deficiencies and dietary habits. Some popular options include:
- Probiotics: These can help maintain gut health and support digestion.
- Omega-3 Fatty Acids: Known for their anti-inflammatory properties.
- Multivitamins: A comprehensive way to fill nutritional gaps.
- Turmeric: Often used for its potential anti-inflammatory effects.
To further illustrate the importance of supplementation, consider the following table outlining common deficiencies and their recommended supplements:
| Nutrient | Common Sources | Recommended Supplement |
|---|---|---|
| Vitamin D | Sunlight, fortified foods | Vitamin D3 |
| Vitamin B12 | Meat, dairy products | B12 Complex |
| Iron | Red meat, legumes | Ferrous Sulfate |
Q&A
Q&A: Navigating the Crohn’s Disease Diet
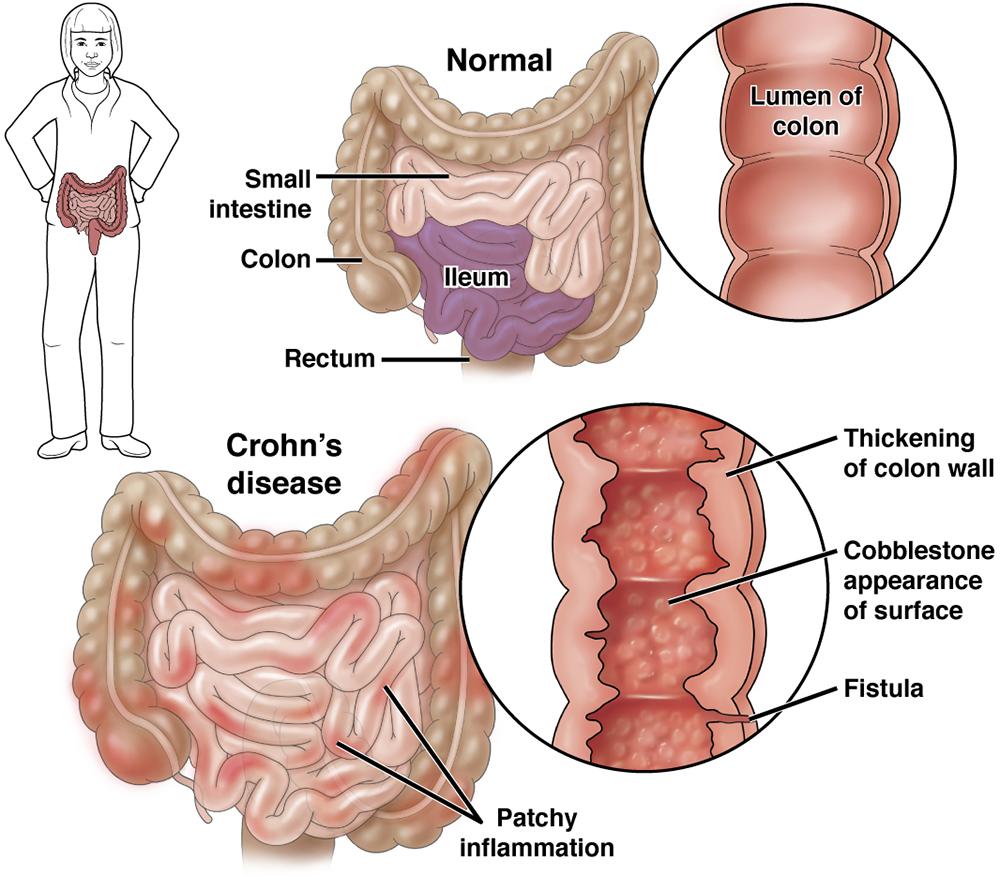
Q1: What exactly is Crohn’s disease, and how does it relate to diet?
A1: Crohn’s disease is a chronic inflammatory condition of the gastrointestinal tract that can cause a variety of symptoms, including abdominal pain, diarrhea, fatigue, and weight loss. While there isn’t a one-size-fits-all diet for those with Crohn’s, certain foods can either exacerbate symptoms or promote healing. Understanding the relationship between diet and Crohn’s is crucial for managing the condition effectively.
Q2: Are there specific foods that people with Crohn’s disease should avoid?
A2: Yes, many people with Crohn’s find that certain foods can trigger symptoms. Common culprits include high-fiber foods, such as raw fruits and vegetables, nuts, and whole grains, as well as dairy products, fatty foods, spicy dishes, and caffeine. It’s essential to listen to your body and identify which foods may be problematic for you.
Q3: What foods are generally considered safe or beneficial for someone with Crohn’s?
A3: While individual tolerances vary, many people with Crohn’s disease find relief with low-fiber foods, such as white rice, plain pasta, and cooked vegetables. Lean proteins like chicken, turkey, and fish can be beneficial, as well as eggs and tofu. Keeping hydration in mind is also important; clear broths and electrolyte-rich drinks can help maintain fluid balance.
Q4: How can someone with Crohn’s disease ensure they are getting enough nutrients?
A4: Nutrient absorption can be a challenge with Crohn’s disease due to inflammation and potential surgeries. To ensure adequate nutrition, consider working with a registered dietitian who specializes in gastrointestinal disorders. They can help create a personalized meal plan that focuses on nutrient-dense foods while accommodating any dietary restrictions.
Q5: Is it important to keep a food diary, and how can it help?
A5: Absolutely! Keeping a food diary can be a valuable tool for managing Crohn’s disease. By documenting what you eat and any symptoms that follow, you can identify patterns and pinpoint trigger foods. This information can empower you to make informed dietary choices and discuss findings with your healthcare team.
Q6: Are there any dietary supplements that might help someone with Crohn’s disease?
A6: Some individuals may benefit from dietary supplements, especially if they’re struggling to get enough nutrients from food alone. Common supplements include multivitamins, vitamin D, calcium, and omega-3 fatty acids. However, it’s essential to consult a healthcare provider before starting any supplements, as they can interact with medications or worsen symptoms.
Q7: Can a Crohn’s disease diet differ during flare-ups versus remission?
A7: Yes, many people with Crohn’s experience different dietary needs depending on their disease status. During flare-ups, a bland, low-fiber diet may be more appropriate to minimize irritation. In remission, individuals might be able to gradually reintroduce a broader range of foods, but it’s important to do so carefully and observe for any returning symptoms.
Q8: What role does stress play in managing a Crohn’s disease diet?
A8: Stress can significantly impact digestive health and exacerbate Crohn’s symptoms. While it’s not directly related to food choices, managing stress through relaxation techniques, meditation, and exercise can complement dietary efforts. By addressing both diet and emotional well-being, individuals can better manage their Crohn’s disease effectively.
This Q&A aims to provide insights into the dietary considerations for those living with Crohn’s disease, highlighting the importance of personalization in food choices and overall health management. Always consult with healthcare professionals for tailored advice.
To Conclude
the journey through Crohn’s disease is often a winding path, filled with challenges and discoveries. As we navigate the intricate relationship between diet and this condition, it becomes clear that what we choose to eat can play a significant role in managing symptoms and enhancing overall well-being. While there is no one-size-fits-all solution, embracing a personalized diet—rich in nutrients and mindful of triggers—can empower individuals to take control of their health.
As you explore various food options and experiment with meals, remember that the key lies in listening to your body and consulting with healthcare professionals. Each plate presents an opportunity for nourishment and healing, and with patience and persistence, you can find the balance that works for you.
Ultimately, the Crohn’s disease diet is not merely a set of restrictions but rather an invitation to explore new flavors, discover wholesome ingredients, and foster a deeper connection with the food that fuels your body. So, as you close this chapter, let it be the beginning of an inspiring culinary adventure—one that honors your health while celebrating the joy of eating.