In the dense thickets of summer woods and grassy fields, where sunlight dances through the leaves and the air is alive with the buzz of nature, a hidden danger lurks: Lyme disease. This tick-borne illness, often masquerading as a simple flu, can lead to a complex web of symptoms that affect the body and mind. As the awareness of Lyme disease grows, so too does the need for effective treatment options that not only alleviate symptoms but also address the root causes of this elusive condition. In this article, we will explore the evolving landscape of Lyme disease treatment, delving into traditional therapies, emerging research, and holistic approaches that offer hope to those affected. Join us as we navigate this intricate journey toward healing, shedding light on a disease that, for many, is more than just a passing concern but a deeply personal battle.
Understanding Lyme Disease and Its Impact on Health
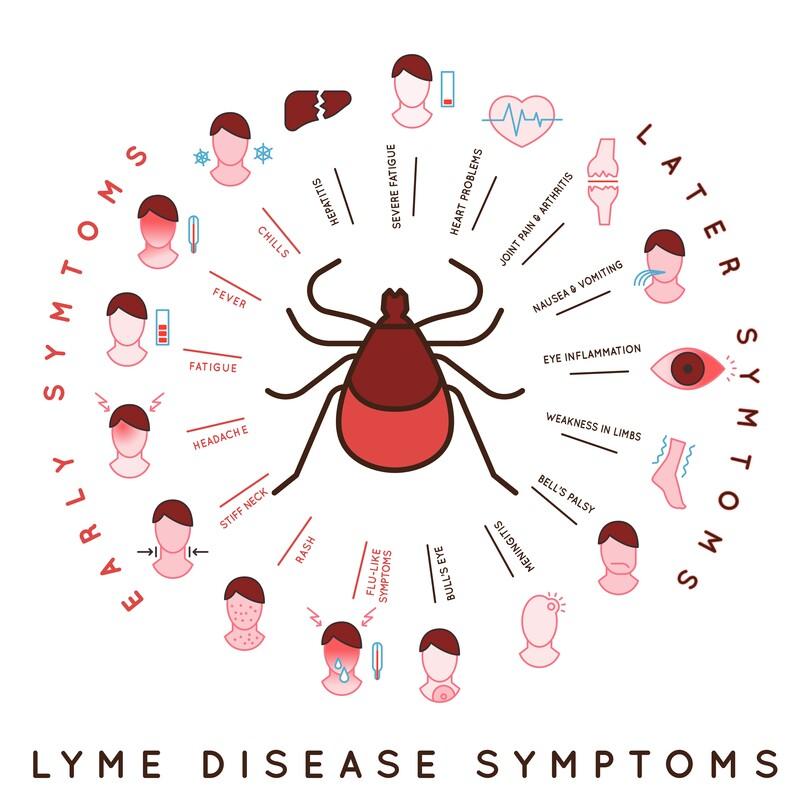
Lyme disease is a complex and multifaceted illness primarily transmitted through the bite of infected black-legged ticks. The disease is caused by the bacterium Borrelia burgdorferi and can lead to a range of symptoms that vary from person to person. Early signs often include fever, headache, fatigue, and a distinctive skin rash known as erythema migrans. If not treated promptly, the infection can progress to more severe manifestations, affecting the joints, heart, and nervous system. This progression can result in long-term health complications that impact an individual’s quality of life significantly.
Addressing Lyme disease requires a comprehensive approach to treatment, focusing not only on eradicating the bacteria but also on managing symptoms. Common treatment options include:
- Antibiotics: The first line of defense, usually prescribed for 10 to 21 days, depending on the severity and stage of the disease.
- Symptomatic relief: Over-the-counter pain relief medications can help manage pain and inflammation.
- Supportive therapies: Physical therapy and lifestyle modifications may play a crucial role in recovery.
For those experiencing lingering symptoms after initial treatment, known as Post-Treatment Lyme Disease Syndrome (PTLDS), managing the condition can be particularly challenging. Research is ongoing to better understand this phenomenon and develop effective strategies. The following table outlines common symptoms associated with PTLDS:
| Symptom | Duration |
|---|---|
| Fatigue | Weeks to months |
| Muscle and joint pain | Ongoing |
| Cognitive difficulties | Variable |
Exploring the Role of Antibiotics in Lyme Disease Treatment
Antibiotics are the cornerstone of Lyme disease treatment, primarily due to their efficacy in combating the spirochete bacterium responsible for the infection, Borrelia burgdorferi. When administered early in the course of the disease, antibiotics can significantly shorten recovery time and reduce the risk of long-term complications. The most commonly prescribed medications include:
- Doxycycline: Effective for adults and children over eight, it not only targets Lyme disease but also offers protection against co-infections.
- Amoxicillin: A suitable alternative for younger children or pregnant women, it provides a favorable safety profile.
- Cefuroxime axetil: Another option for those who may not tolerate doxycycline or amoxicillin.
While most patients respond well to a standard treatment regimen, it’s crucial to monitor for any residual symptoms. Some individuals may experience persistent issues even after antibiotic therapy, a condition often referred to as Post-Treatment Lyme Disease Syndrome (PTLDS). Researchers are exploring various factors contributing to this phenomenon, including:
- Immune response:** Differences in individual immune responses may lead to prolonged symptoms.
- Co-infections: The presence of other tick-borne infections can complicate recovery.
- Antibiotic resistance: Some strains of the bacteria may develop resistance, limiting treatment effectiveness.
| Antibiotic | Duration of Treatment | Common Side Effects |
|---|---|---|
| Doxycycline | 10-21 days | Nausea, sensitivity to sunlight |
| Amoxicillin | 14-21 days | Diarrhea, rash |
| Cefuroxime axetil | 14-21 days | Fatigue, headache |
Complementary Therapies for Managing Symptoms
Managing the symptoms of Lyme disease can be challenging, and many individuals find that incorporating complementary therapies into their treatment plan offers relief. These therapies often focus on holistic approaches, enhancing overall well-being while addressing the specific symptoms associated with the disease. Some effective complementary therapies include:
- Acupuncture: This ancient practice can help reduce pain and inflammation, promoting relaxation.
- Meditation and Mindfulness: These techniques can alleviate stress and improve mental clarity, which is crucial for those battling chronic symptoms.
- Nutritional Therapy: A diet rich in anti-inflammatory foods can support the immune system and overall recovery.
- Herbal Remedies: Certain herbs, like cat’s claw and astragalus, are believed to have properties that combat Lyme disease.
In addition to these therapies, engaging in gentle physical activities such as yoga or tai chi can enhance physical function and boost mood. Many people also benefit from supportive practices that foster emotional health, such as counseling or support groups. Here’s a quick overview of some holistic treatment options:
| Therapy | Benefits |
|---|---|
| Acupuncture | Reduces pain and promotes relaxation |
| Meditation | Reduces stress and enhances focus |
| Nutritional Therapy | Supports immune function and reduces inflammation |
| Herbal Remedies | May help combat disease symptoms |
The Importance of Early Diagnosis in Successful Treatment
Early detection of Lyme disease significantly influences the efficacy of treatment methods. When diagnosed promptly, patients have a higher chance of overcoming the disease with minimal complications. Symptoms like fever, fatigue, and the characteristic bull’s-eye rash often appear within the first few weeks of infection. Identifying these signs early allows for quick intervention, which can include:
- Antibiotic therapy: Typically prescribed for 10 to 21 days.
- Symptom management: Addressing pain and fatigue through various approaches.
- Regular monitoring: Ensuring the effectiveness of treatment and making adjustments as needed.
In contrast, delayed diagnosis can lead to severe complications, as the bacteria can spread to the joints, heart, and nervous system. The progression from early localized Lyme disease to more advanced stages can result in chronic symptoms that are harder to treat. To illustrate the potential consequences of delayed diagnosis, consider the following:
| Stage of Lyme Disease | Typical Symptoms | Potential Complications |
|---|---|---|
| Early Localized | Rash, fatigue, headache | Minimal |
| Early Disseminated | Joint pain, neurological issues | Long-term joint damage |
| Late Disseminated | Neuropathy, chronic arthritis | Severe impairment in daily activities |
Preventive Strategies to Reduce the Risk of Infection
Reducing the risk of infection is crucial for anyone living in or visiting areas known for Lyme disease. Implementing simple yet effective preventive measures can make a significant difference. Here are some important strategies to consider:
- Wear Protective Clothing: Opt for long sleeves and pants, especially when venturing into wooded or grassy areas. Light-colored clothing can help you spot ticks more easily.
- Use Tick Repellents: Apply insect repellent containing DEET or permethrin on clothing and exposed skin to deter ticks.
- Check for Ticks Regularly: Conduct thorough tick checks on yourself, your pets, and children after outdoor activities to catch any ticks before they attach.
- Maintain Your Yard: Keep your lawn mowed, remove leaf litter, and create barriers with gravel or wood chips to reduce tick habitats.
- Shower After Outdoor Activities: Showering within two hours of being outdoors can help wash away ticks before they attach.
In addition to these personal preventive measures, community awareness and action play a vital role in reducing Lyme disease risks. Educational programs can help inform the public about the signs of Lyme disease and the importance of prevention. Consider supporting local initiatives or even organizing community clean-up days to eliminate potential tick habitats. The following table highlights key community practices:
| Practice | Description |
|---|---|
| Community Awareness Campaigns | Educate residents about tick prevention and Lyme disease symptoms. |
| Regular Park Maintenance | Keep parks and recreational areas clean and well-maintained to minimize tick habitats. |
| Collaborative Research | Support studies that aim to improve understanding of Lyme disease and its prevention. |
Navigating Post-Treatment Lyme Disease Syndrome and Recovery Options
After the initial treatment for Lyme disease, some individuals may experience lingering symptoms known as Post-Treatment Lyme Disease Syndrome (PTLDS). This complex condition can include a variety of issues such as fatigue, muscle and joint pain, cognitive difficulties, and sleep disturbances. Those facing PTLDS often find it challenging to return to their pre-illness state. It’s essential for patients to approach recovery holistically, engaging with a multidisciplinary team that may include physicians, physical therapists, and mental health professionals. Understanding the multifaceted nature of PTLDS can empower patients to seek tailored strategies that address both physical and emotional well-being.
Recovery options for PTLDS can vary significantly from person to person, and it’s crucial for patients to explore different avenues to find what works best for them. Some effective methods include:
- Physical Therapy: A tailored exercise regimen can help alleviate pain and improve mobility.
- Cognitive Behavioral Therapy: This can address emotional challenges and promote coping strategies.
- Nutrition and Supplements: A balanced diet and certain supplements may support the immune system and overall health.
- Mindfulness and Meditation: Techniques like yoga and meditation can help manage stress and improve mental clarity.
Patients may also benefit from tracking their symptoms and recovery progress through a structured approach. Below is a simple table that can help individuals monitor their well-being and identify potential triggers:
| Date | Symptom Severity (1-10) | Activities | Notes |
|---|---|---|---|
| MM/DD/YYYY | 7 | Light exercise, meditation | Felt fatigued after activities |
| MM/DD/YYYY | 5 | Yoga session | Improved mood, less pain |
| MM/DD/YYYY | 6 | Social outing | Enjoyed but exhausted afterward |
Incorporating these strategies into a daily routine can create a supportive environment for recovery and enhance the quality of life. Regular communication with healthcare providers is essential to adapt recovery plans as needed, ensuring a comprehensive approach to managing PTLDS.
Q&A
Q&A: Understanding Lyme Disease Treatment
Q1: What is Lyme disease, and how is it contracted?
A1: Lyme disease is an infectious illness caused by the Borrelia bacteria, primarily transmitted to humans through the bite of infected black-legged ticks, often referred to as deer ticks. The disease is most commonly found in wooded and grassy areas, where these ticks thrive. Recognizing the risk factors, particularly during outdoor activities in affected regions, is crucial for prevention.
Q2: What are the common symptoms of Lyme disease?
A2: Symptoms of Lyme disease can vary widely, but they often begin with a characteristic circular rash resembling a “bull’s-eye” at the site of the tick bite, which can appear within days to weeks. Other early symptoms may include fever, chills, fatigue, headaches, and muscle or joint aches. If left untreated, Lyme disease can progress to more severe symptoms, affecting the heart, joints, and nervous system.
Q3: How is Lyme disease diagnosed?
A3: Diagnosis typically involves a combination of a physical examination, patient history, and specific laboratory tests. Healthcare providers may look for the classic rash and inquire about potential exposure to ticks. Blood tests can also detect antibodies to the Borrelia bacteria, though these may take several weeks to develop after infection.
Q4: What are the primary treatment options for Lyme disease?
A4: The standard treatment for Lyme disease usually consists of antibiotics, which are most effective when started early in the infection. Doxycycline, amoxicillin, and cefuroxime axetil are commonly prescribed options, typically administered for 10 to 21 days depending on the stage of the disease and the patient’s symptoms. Most patients respond well to these treatments and see significant improvement.
Q5: Are there any alternative treatments for Lyme disease?
A5: While some individuals may explore alternative or complementary therapies, it is essential to approach these options with caution. Treatments such as herbal remedies, dietary changes, and acupuncture may provide supportive care, but they should not replace conventional medical treatment. Discussing any alternative options with a healthcare provider is important to ensure a coordinated and safe approach to care.
Q6: What are the potential complications of Lyme disease if left untreated?
A6: If Lyme disease is not treated promptly, it can lead to severe complications, including Lyme arthritis, characterized by swelling and pain in the joints, particularly the knees. It may also affect the heart, causing Lyme carditis, which can result in heart palpitations or other cardiovascular issues. Neurological complications, such as meningitis or facial palsy, can also arise, underscoring the importance of early diagnosis and treatment.
Q7: How can one prevent Lyme disease?
A7: Prevention is key to avoiding Lyme disease. Individuals can reduce their risk by wearing protective clothing, using insect repellent with DEET, and performing thorough tick checks after spending time outdoors. Keeping yards tidy, maintaining a tick-free environment, and being mindful of the seasons when ticks are most active can further diminish exposure.
Q8: Is there a vaccine for Lyme disease?
A8: As of now, there is no widely available vaccine for Lyme disease for humans. However, research is ongoing to develop a vaccine that could protect against the disease. Meanwhile, preventive measures and awareness remain critical in reducing the incidence of Lyme disease.
Q9: What should someone do if they suspect they have Lyme disease?
A9: If you suspect you have Lyme disease, it’s important to consult a healthcare provider as soon as possible. Early intervention significantly increases the likelihood of a full recovery. Be prepared to discuss any recent outdoor activities, tick exposure, and any symptoms you may have experienced, as this information can assist in diagnosis and treatment planning.
Q10: What is the outlook for individuals diagnosed with Lyme disease?
A10: The prognosis for individuals diagnosed with Lyme disease is generally positive, especially when treated early. Most patients recover fully with appropriate antibiotic therapy. However, some may experience lingering symptoms, a condition sometimes referred to as Post-Treatment Lyme Disease Syndrome (PTLDS). Ongoing research is focused on understanding this condition and improving care for affected individuals.
To Conclude
As we navigate the intricate landscape of Lyme disease treatment, it becomes clear that a multifaceted approach is essential for effective management and recovery. From early detection to personalized treatment plans, the journey of healing is as unique as each individual affected by this tick-borne illness.
As research continues to evolve, so too does our understanding of the nuances of Lyme disease, offering hope for those in the grip of its persistent symptoms. Empowered by knowledge, patients can advocate for their health, collaborate with healthcare providers, and explore the diverse avenues of care available to them.
the fight against Lyme disease is not solely a battle of science and medicine; it is also a testament to resilience, community support, and the unwavering human spirit. As you close this chapter on Lyme disease treatment, may you carry with you a sense of hope and a commitment to staying informed, for in awareness lies the power to embrace healing and reclaim one’s life from the shadows of illness.