Title: Navigating the Maze of Irritable Bowel Syndrome Treatments
Introduction:
For millions around the globe, the battle with Irritable Bowel Syndrome (IBS) is an ongoing struggle, marked by unpredictable flare-ups and discomfort that can disrupt even the simplest of daily routines. As a condition that remains shrouded in mystery, IBS often defies easy categorization and treatment. Yet, within this complexity lies a wealth of knowledge and an array of therapeutic options tailored to alleviate symptoms and improve quality of life. In this article, we will embark on a journey through the diverse landscape of IBS treatments, exploring everything from dietary adjustments and lifestyle changes to medication and alternative therapies. Whether you are newly diagnosed or seeking to refine your current management plan, our guide aims to illuminate the possibilities and empower you to take control of your digestive well-being.
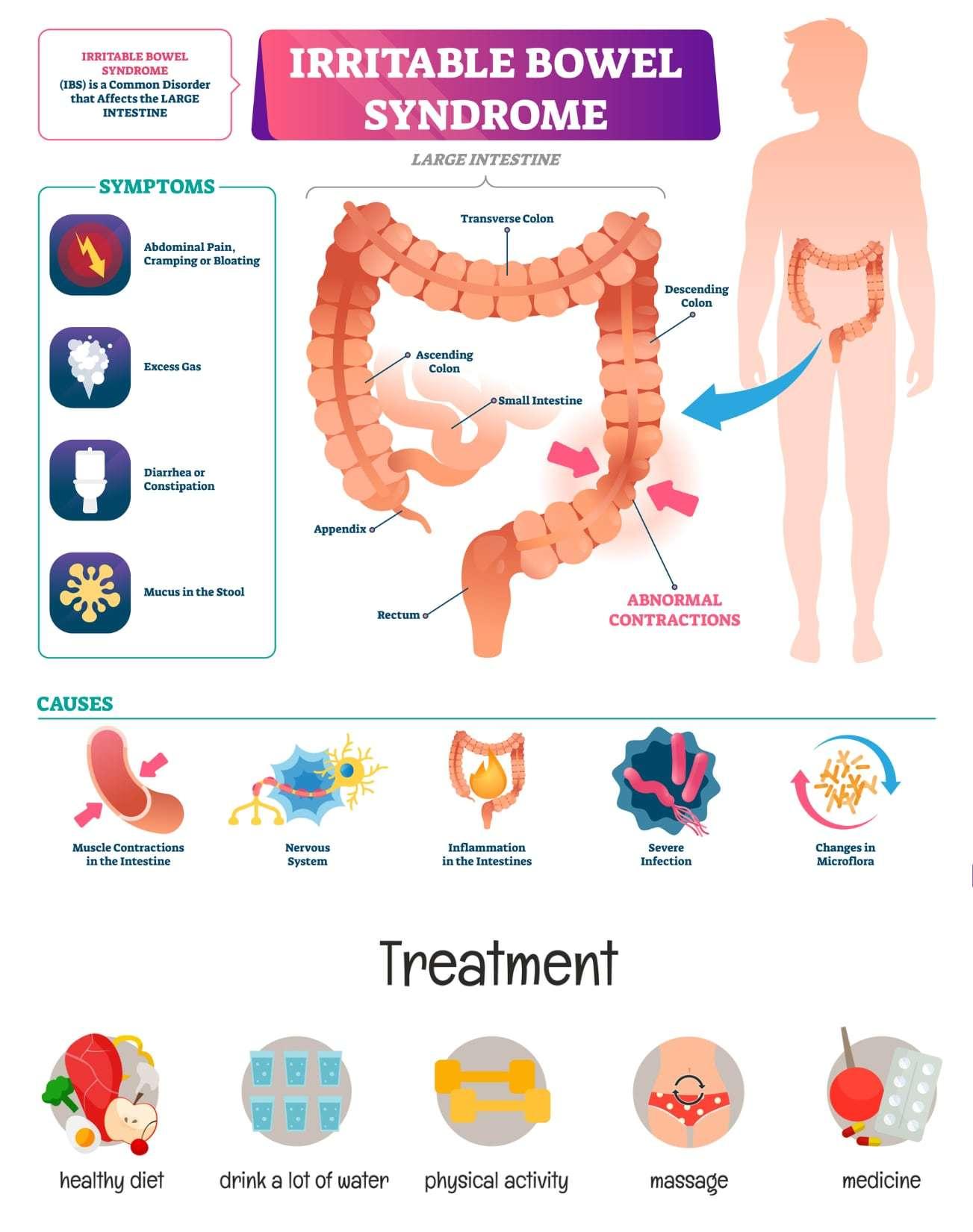
Understanding Irritable Bowel Syndrome and Its Impact on Daily Life
Irritable Bowel Syndrome (IBS) is a complex gastrointestinal disorder that affects millions of people worldwide. Its symptoms, which include abdominal pain, bloating, gas, and irregular bowel movements, can significantly disrupt daily activities and overall quality of life. Individuals often find themselves navigating a minefield of triggers, particularly when it comes to diet and stress management. Common triggers for IBS flare-ups can include:
- High-fat foods
- Caffeine
- Alcohol
- Stress
- Large meals
Living with IBS requires not only recognizing these triggers but also implementing practical strategies to minimize their impact. Treatment options vary widely, often tailored to individual symptoms and lifestyle needs. Many find relief through dietary adjustments, such as adopting a low FODMAP diet, which eliminates specific fermentable carbohydrates known to exacerbate symptoms. Additionally, some may benefit from medications, psychotherapy, or alternative therapies such as acupuncture. Below is a brief overview of popular treatment options:
| Treatment Option | Description |
|---|---|
| Dietary Changes | Adopting a low FODMAP diet to identify and avoid trigger foods. |
| Medications | Prescription or over-the-counter medications to manage symptoms. |
| Psychotherapy | Cognitive-behavioral therapy to address stress and anxiety. |
| Alternative Therapies | Acupuncture and relaxation techniques to alleviate symptoms. |
Dietary Adjustments: Foods to Embrace and Avoid for Relief
Managing irritable bowel syndrome (IBS) often requires a careful examination of dietary choices. Those suffering from this condition can find significant relief by embracing foods that promote gut health and avoiding those that trigger discomfort. Consider incorporating the following options into your meals:
- Soluble fiber-rich foods: Oats, apples, and carrots can help regulate bowel movements.
- Lean proteins: Skinless poultry, fish, and eggs are gentle on the digestive system.
- Low-FODMAP fruits: Bananas, blueberries, and strawberries can be beneficial.
- Fermented foods: Yogurt, kefir, and sauerkraut may aid in gut health.
Conversely, certain foods are known to exacerbate IBS symptoms and should be minimized or avoided altogether. These include:
- High-FODMAP foods: Garlic, onions, and wheat products can lead to bloating and discomfort.
- Fatty and fried foods: These can be hard to digest and may trigger spasms.
- Dairy products: For those who are lactose intolerant, these can cause significant issues.
- Artificial sweeteners: Sorbitol and mannitol are known to provoke gastrointestinal distress.
To provide a clearer understanding of the foods to embrace versus those to avoid, here’s a simple comparison:
| Foods to Embrace | Foods to Avoid |
|---|---|
| Oats | Garlic |
| Fish | Onions |
| Bananas | Wheat |
| Yogurt | Fatty meats |
The Role of Stress Management in IBS Treatment Strategies
Managing stress is a critical component in the treatment of irritable bowel syndrome (IBS), as the mind-body connection plays a significant role in gastrointestinal health. Stress can exacerbate symptoms such as abdominal pain, bloating, and diarrhea by triggering the gut-brain axis. Therefore, incorporating effective stress management techniques can lead to substantial improvements in the quality of life for those suffering from IBS. Some of the most beneficial strategies include:
- Mindfulness Meditation: Practicing mindfulness helps individuals stay present and reduces anxiety, which can alleviate IBS symptoms.
- Yoga and Physical Activity: Regular exercise promotes digestive health and releases endorphins, mitigating stress levels.
- Cognitive Behavioral Therapy (CBT): This therapy can reshape negative thought patterns that contribute to stress and IBS flare-ups.
- Breathing Techniques: Deep breathing can activate the body’s relaxation response, helping to calm an overactive gut.
Integrating these stress management strategies into an IBS treatment plan not only addresses the physical aspects of the syndrome but also fosters emotional well-being. Personalized approaches can vary from one individual to another, so it’s essential to find the right mix of techniques that resonate. Additionally, tracking stress levels alongside IBS symptoms can help health professionals tailor treatment more effectively. Here’s a simple table summarizing common stress management techniques and their benefits:
| Technique | Benefit |
|---|---|
| Mindfulness Meditation | Reduces anxiety and enhances focus |
| Yoga | Improves flexibility and promotes relaxation |
| Cognitive Behavioral Therapy | Addresses negative thought patterns |
| Breathing Techniques | Activates relaxation response |
Medications and Supplements: Exploring Options for Symptom Control
Managing the symptoms of irritable bowel syndrome (IBS) can often feel like navigating a maze, and for many, medications and supplements are key tools in finding relief. Traditional medications prescribed by healthcare providers may include antispasmodics, which help reduce cramping, and antidiarrheals for those experiencing diarrhea. Additionally, laxatives can be beneficial for individuals suffering from constipation. On the other hand, some may find comfort in over-the-counter options such as fiber supplements and probiotics, which can help regulate bowel movements and promote gut health. The choice of treatment largely depends on individual symptoms and responses, so collaborating with a healthcare professional is crucial.
In recent years, a variety of supplements have emerged as popular alternatives or complementary options to traditional medications. Consider the following options:
- Peppermint oil – Known for its soothing effects on the digestive tract.
- L-glutamine – An amino acid that supports gut lining integrity.
- Digestive enzymes – Aid in breaking down food for better absorption and reduced bloating.
- Turmeric – Contains curcumin, which may help alleviate inflammation in the gut.
Before embarking on any supplement regimen, it’s important to consider potential interactions with existing medications. The following table summarizes common medications and their potential interactions with popular supplements:
| Medication | Potential Interaction with Supplement |
|---|---|
| Antispasmodics | May interact with peppermint oil, leading to enhanced effects. |
| Antidiarrheals | Turmeric may reduce effectiveness if taken together. |
| Laxatives | Fiber supplements may enhance laxative effects. |
| Probiotics | Generally safe; may enhance the effects of digestive enzymes. |
Alternative Therapies: Integrating Mind-Body Approaches in IBS Care
In the quest to manage irritable bowel syndrome (IBS), many individuals are turning to alternative therapies that focus on the intricate connection between the mind and body. These approaches can complement traditional treatments, offering holistic benefits that address not just the physical symptoms but also the emotional and psychological aspects of living with IBS. Popular mind-body practices include:
- Mindfulness Meditation: This practice helps individuals center their thoughts, reduce stress, and promote a sense of calm, which can alleviate IBS symptoms.
- Yoga: Incorporating gentle movements and breath control, yoga facilitates relaxation and improves digestive function.
- Biofeedback: This technique teaches awareness and control over physiological functions, empowering patients to manage their IBS symptoms effectively.
Integrating these therapies into IBS care not only supports gastrointestinal health but also fosters emotional resilience. A growing body of evidence suggests that patients who engage in mind-body techniques may experience improved symptom management and a better quality of life. The following table highlights key benefits of these approaches:
| Therapy | Benefits |
|---|---|
| Mindfulness Meditation | Reduces anxiety, improves focus. |
| Yoga | Enhances flexibility, promotes relaxation. |
| Biofeedback | Increases awareness, fosters self-regulation. |
Personalized Treatment Plans: Tailoring Approaches to Individual Needs
Managing irritable bowel syndrome (IBS) effectively often requires personalized treatment plans that focus on the unique needs of each individual. Since IBS symptoms can vary widely from person to person, a one-size-fits-all approach may not yield the desired results. To create an effective management strategy, healthcare providers might consider a combination of dietary modifications, lifestyle changes, and therapeutic options tailored to the patient’s specific symptoms and triggers. This comprehensive approach allows for gradual adjustments, ensuring that patients can monitor their responses and refine their treatment as needed.
Some of the key elements that may be included in a personalized IBS treatment plan are:
- Dietary adjustments: Identifying food intolerances, such as gluten or lactose, and incorporating a low-FODMAP diet.
- Medications: Exploring options like antispasmodics or laxatives based on symptom presentation.
- Stress management: Integrating techniques such as yoga or mindfulness to alleviate stress-induced symptoms.
- Regular exercise: Encouraging physical activity to enhance overall gastrointestinal health.
By collaborating closely with healthcare professionals, individuals can monitor their progress and adapt their treatment plans, ensuring they align with their evolving needs. The goal is to empower patients to take control of their IBS and improve their quality of life through meaningful and targeted interventions.
Q&A
Q&A: Navigating the Maze of Irritable Bowel Syndrome Treatments
Q1: What exactly is Irritable Bowel Syndrome (IBS) and what are its common symptoms?
A1: Irritable Bowel Syndrome, commonly known as IBS, is a gastrointestinal disorder that affects the large intestine. It’s characterized by a variety of symptoms, including abdominal pain, bloating, gas, diarrhea, and constipation. The symptoms can vary widely from person to person and may fluctuate in intensity, making IBS a complex condition to manage.
Q2: What are the main treatment approaches for IBS?
A2: There’s no one-size-fits-all treatment for IBS, but a combination of dietary changes, lifestyle adjustments, and medications can help manage symptoms. Common approaches include:
- Dietary Modifications: Many find relief by adopting diets such as the Low FODMAP diet, which reduces certain fermentable carbohydrates that can exacerbate symptoms.
- Medications: Depending on symptoms, doctors may prescribe antidiarrheal medications, laxatives, or even medications specifically approved for IBS, like rifaximin or lubiprostone.
- Stress Management: Since stress can exacerbate IBS symptoms, techniques such as mindfulness, yoga, or therapy can be beneficial.
Q3: How important is diet in managing IBS?
A3: Diet plays a crucial role in managing IBS. Identifying food triggers and adjusting one’s diet accordingly can lead to significant symptom relief. Many patients benefit from keeping a food diary to track what they eat and how their bodies respond. Additionally, the Low FODMAP diet has gained popularity for its effectiveness in reducing symptoms by eliminating fermentable sugars that can cause bloating and discomfort.
Q4: Are there any natural remedies that can help with IBS?
A4: Yes, several natural remedies may provide relief for IBS sufferers. Probiotics, which promote a healthy gut microbiome, can be beneficial. Herbal teas, such as peppermint and ginger, are known for their soothing properties and may help with digestion. However, it’s crucial to consult with a healthcare provider before trying new remedies to ensure they’re appropriate for your specific symptoms.
Q5: Is it possible for IBS symptoms to worsen over time?
A5: While IBS is typically viewed as a chronic condition, symptoms can fluctuate and evolve. Stress, dietary changes, and other health issues can influence symptom severity. Regular check-ins with a healthcare provider can help in adjusting treatment plans as needed to manage worsening symptoms effectively.
Q6: How can I work with my healthcare provider to manage IBS?
A6: Collaboration with your healthcare provider is key to effectively managing IBS. Open communication about your symptoms, triggers, and any changes in your condition is essential. Together, you can explore various treatment options, adjust medications, and monitor your progress. Keeping a symptom diary can be a valuable tool in these discussions, providing insights that can help tailor your treatment plan.
Q7: Are there any support groups or resources for IBS patients?
A7: Absolutely! Many organizations, such as the International Foundation for Gastrointestinal Disorders (IFFGD) and the IBS Network, offer valuable resources, support groups, and educational materials. Engaging with others who understand the challenges of living with IBS can provide emotional support and practical tips for managing the condition.
By understanding the intricacies of IBS treatments and maintaining an open dialogue with healthcare providers, individuals can navigate their journey to symptom relief more effectively. Remember, while IBS can be a challenging condition, there are numerous avenues to explore for managing symptoms and enhancing quality of life.
Wrapping Up
navigating the complexities of irritable bowel syndrome can feel like traversing a winding road filled with unexpected turns. However, with a wealth of treatment options at your disposal—from dietary adjustments and lifestyle changes to medication and alternative therapies—there lies a spectrum of hope for those affected. Each individual’s journey is unique, and what works for one may not work for another. Therefore, it’s essential to approach your treatment plan with patience and an open mind, collaborating closely with healthcare professionals who understand your specific needs. Armed with knowledge and a proactive attitude, you can take charge of your well-being, transforming challenges into manageable solutions. Remember, while IBS may be a part of your life, it doesn’t define you, and a brighter, more comfortable future is within reach.