Understanding Type 2 Diabetes: Navigating the Complex Landscape of a Modern Epidemic
In a world where lifestyle choices often collide with genetic predispositions, type 2 diabetes has emerged as one of the most pressing health challenges of our time. Once primarily associated with adults, this chronic condition increasingly affects younger populations, raising questions about diet, activity levels, and the very fabric of our daily lives. As we delve into the intricacies of type 2 diabetes, we will explore its biological underpinnings, the risk factors that contribute to its prevalence, and the multitude of strategies available for prevention and management. This article aims to illuminate the path to understanding and addressing a condition that impacts millions globally, offering insights that empower both individuals and communities in the fight against diabetes. Join us as we unpack the complexities of this modern epidemic and seek to foster a greater awareness of its implications for health and well-being.
Understanding the Roots of Type 2 Diabetes and Its Risk Factors
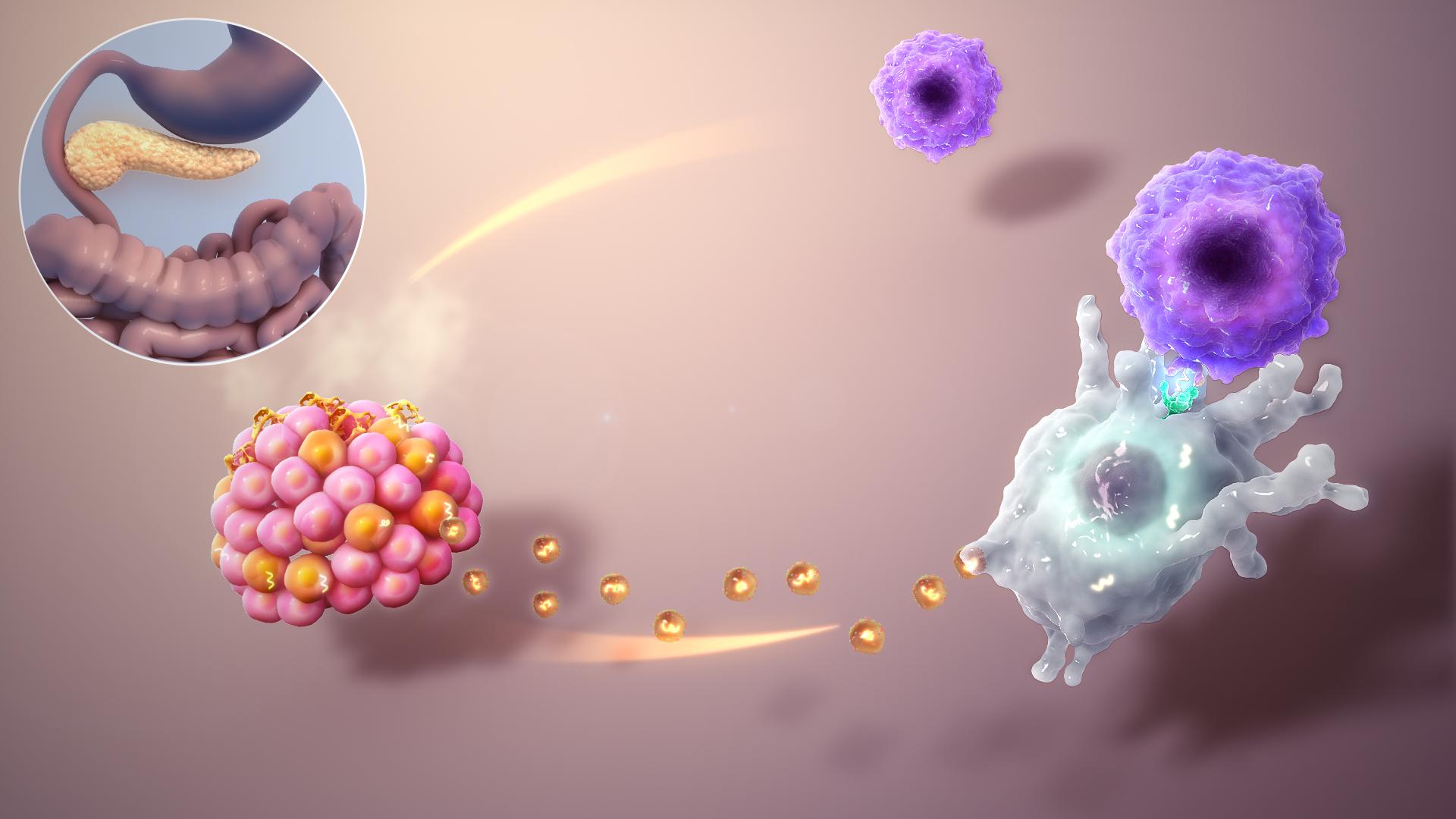
Type 2 diabetes is a complex metabolic disorder that primarily arises from insulin resistance, where the body’s cells fail to respond effectively to insulin. This condition often develops gradually and can be influenced by a combination of genetic and environmental factors. Key risk factors associated with the onset of type 2 diabetes include:
- Obesity: Excess body fat, particularly around the abdomen, is a significant contributor.
- Physical Inactivity: A sedentary lifestyle diminishes insulin sensitivity.
- Unhealthy Diet: High consumption of processed foods and sugars can lead to weight gain and metabolic issues.
- Age: Risk increases as individuals age, especially after 45 years.
- Family History: A genetic predisposition can elevate the likelihood of developing the disease.
Aside from these major factors, other emerging contributors to type 2 diabetes have been identified. For instance, sleep disorders, such as sleep apnea, can significantly affect insulin sensitivity and glucose metabolism. Moreover, chronic stress has been shown to increase cortisol levels, which can make it more challenging for the body to maintain normal blood sugar levels. Understanding the intricate interplay of these elements is crucial in formulating effective prevention and management strategies. The following table highlights additional risk factors:
| Risk Factor | Impact |
|---|---|
| Gestational Diabetes | Increases risk for future diabetes |
| High Blood Pressure | Linked with insulin resistance |
| Low HDL Cholesterol | Raises diabetes risk |
| Polycystic Ovary Syndrome (PCOS) | Associated with insulin resistance |
Nourishing Choices: A Deep Dive into Diet and Nutrition for Diabetes Management
Managing type 2 diabetes is not solely about medication; it is deeply intertwined with diet and nutrition. A well-planned diet can help maintain blood glucose levels within a target range, thus mitigating the risk of complications. Here are some key dietary strategies to consider:
- Emphasize whole foods: Fill your plate with vegetables, fruits, whole grains, and lean proteins.
- Control portion sizes: Be mindful of serving sizes to prevent overeating.
- Monitor carbohydrate intake: Understand the impact of carbs on blood sugar levels and choose complex carbohydrates.
- Stay hydrated: Drink plenty of water throughout the day to stay hydrated without added sugars.
Creating a balanced meal plan can help you make informed choices while enjoying a variety of foods. Below is a simple table showcasing recommended foods and their benefits for individuals managing type 2 diabetes:
| Food Item | Benefit |
|---|---|
| Leafy Greens | Low in calories, high in nutrients and fiber. |
| Fatty Fish | Rich in omega-3 fatty acids, promoting heart health. |
| Legumes | High in protein and fiber, helping to stabilize blood sugar. |
| Whole Grains | Provide essential nutrients and help maintain steady energy levels. |
The Power of Movement: Exercise Strategies to Combat Type 2 Diabetes
Engaging in regular physical activity is a powerful tool in managing type 2 diabetes. Exercise not only aids in weight loss but also enhances insulin sensitivity, allowing your body to use glucose more effectively. Incorporating a mix of aerobic exercises and strength training can yield significant benefits. Aim for at least 150 minutes of moderate-intensity aerobic activity each week, such as brisk walking, cycling, or swimming. Additionally, incorporating strength training exercises twice a week can help build muscle, which plays a critical role in glucose metabolism.
Making exercise a part of your daily routine doesn’t have to be overwhelming. Here are some effective strategies to get started:
- Set realistic goals: Begin with short sessions and gradually increase duration and intensity.
- Find activities you enjoy: Dancing, hiking, or group classes can make exercise more enjoyable.
- Stay consistent: Schedule workouts like appointments to establish a routine.
- Incorporate movement into your day: Take the stairs, walk during lunch breaks, or do household chores.
Mindful Living: Stress Management Techniques for Better Blood Sugar Control
Incorporating mindfulness into your daily routine can significantly improve your ability to manage stress, which in turn supports better blood sugar control. The practice of mindfulness encourages a heightened awareness of the present moment, allowing individuals with type 2 diabetes to respond to stressors more effectively. Some practical techniques include:
- Breathing Exercises: Spend a few minutes focusing on your breath. Inhale deeply through your nose, hold for a moment, and exhale slowly through your mouth. This simple act can lower cortisol levels, the stress hormone that may impact blood sugar.
- Mindful Eating: Pay attention to each bite you take. Savor the flavors and textures of your food, which can help regulate your appetite and portion sizes.
- Daily Meditation: Set aside time each day to meditate. Even short sessions can clear your mind and reduce anxiety.
Another powerful tool in stress management is physical activity, which can further enhance blood sugar control. Engaging in regular exercise releases endorphins, which help alleviate stress and improve mood. Consider the following activities:
- Walking: A brisk 30-minute walk can serve both as a form of exercise and a time for mindfulness, allowing you to connect with nature.
- Yoga: This practice combines physical movement with breath control, perfect for cultivating a sense of inner peace while also improving flexibility and strength.
- Nature Therapy: Spending time outdoors can be rejuvenating. Try to find a serene environment to promote relaxation and mindfulness.
Monitoring Progress: Essential Tools for Tracking Diabetes Health
Maintaining optimal health with type 2 diabetes involves consistent monitoring and the use of various tools to track crucial metrics. Here are some essential tools that can empower individuals managing their diabetes:
- Blood Glucose Meters: These handheld devices allow users to check their blood sugar levels at home. Regular testing helps in adjusting diet and medication as needed.
- Continuous Glucose Monitors (CGMs): CGMs provide real-time glucose readings throughout the day, offering insights into how food, activity, and medication affect blood sugar levels.
- Diabetes Management Apps: Mobile applications can help log blood glucose readings, track meals, and set reminders for medication, fostering better organization and accountability.
- Wearable Fitness Trackers: Devices like smartwatches can monitor physical activity, sleep patterns, and heart rate, aiding in a comprehensive approach to health management.
Having the right tools is only part of the solution; understanding how to interpret the data they provide is equally important. Below is a simple table highlighting key metrics to monitor for effective diabetes management:
| Metric | Recommended Range |
|---|---|
| Fasting Blood Sugar | 70-130 mg/dL |
| Post-Meal Blood Sugar | Less than 180 mg/dL |
| A1C Level | Below 7% |
By utilizing these tools and understanding key health metrics, individuals can take charge of their diabetes management and work towards a healthier future.
Building a Support System: The Role of Community and Professional Guidance in Diabetes Care
Living with type 2 diabetes can be a challenging journey, but having a robust support system can make all the difference. A nurturing community provides not only emotional backing but also practical resources that help individuals navigate their daily lives with diabetes. This can include family, friends, support groups, and online forums where people share their experiences and coping strategies. By surrounding oneself with understanding and empathetic individuals, diabetes management becomes less isolating and more collaborative. Key benefits of a supportive community include:
- Shared Experiences: Learning from others who face similar challenges can offer new insights and encouragement.
- Moral Support: Having someone to talk to during tough times can ease feelings of anxiety and frustration.
- Accountability: Friends and peers can motivate each other to stick to healthy habits and treatment plans.
In addition to community support, seeking professional guidance is equally crucial for effective diabetes care. Healthcare providers, including endocrinologists, nutritionists, and diabetes educators, offer personalized strategies based on individual health profiles. Their expertise not only aids in creating effective management plans but also ensures that patients stay informed about the latest developments in diabetes care. Regular consultations with healthcare professionals can cover important aspects such as:
| Focus Area | Importance |
|---|---|
| Nutrition | Tailored meal plans to maintain stable blood sugar levels. |
| Medication Management | Adjusting dosages and types of medications to optimize treatment. |
| Regular Monitoring | Tracking blood sugar levels to identify patterns and make timely adjustments. |
Q&A
Q&A on Type 2 Diabetes: Understanding the Basics
Q1: What is type 2 diabetes?
A: Type 2 diabetes is a chronic condition that affects the way your body metabolizes sugar (glucose), an essential source of fuel for your body. Unlike type 1 diabetes, where the body fails to produce insulin, type 2 diabetes involves insulin resistance, meaning the body doesn’t use insulin effectively. Over time, the pancreas can’t keep up with the increased demand for insulin, leading to elevated blood sugar levels.
Q2: What are the common symptoms of type 2 diabetes?
A: Common symptoms include increased thirst, frequent urination, extreme fatigue, blurred vision, slow-healing sores, and unexplained weight loss. Some people may not experience noticeable symptoms, which is why regular screening is vital, especially for those at higher risk.
Q3: Who is at risk for developing type 2 diabetes?
A: Several factors can increase the risk of developing type 2 diabetes. These include age (risk increases after 45), obesity, a sedentary lifestyle, family history, and certain ethnic backgrounds. Additionally, conditions like high blood pressure and high cholesterol can also elevate risk.
Q4: How is type 2 diabetes diagnosed?
A: Type 2 diabetes can be diagnosed through several tests. A fasting blood sugar test, an A1C test (which measures average blood sugar levels over the past 2-3 months), or an oral glucose tolerance test can help determine if someone has diabetes. The results will help healthcare professionals develop a tailored management plan.
Q5: What lifestyle changes can help manage or prevent type 2 diabetes?
A: Adopting a healthy lifestyle can make a significant difference. This includes maintaining a balanced diet rich in whole grains, vegetables, and lean proteins, engaging in regular physical activity, managing weight, and avoiding tobacco use. Small changes, like swapping sugary drinks for water or taking the stairs instead of the elevator, can add up over time.
Q6: Can type 2 diabetes be reversed?
A: While “reversal” isn’t a guaranteed outcome, many individuals can achieve normal blood sugar levels through significant lifestyle changes. Weight loss, a nutritious diet, and consistent exercise can help some people reduce their reliance on medication and manage their condition effectively.
Q7: How is type 2 diabetes treated?
A: Treatment for type 2 diabetes often begins with lifestyle modifications. If blood sugar levels remain high, medication may be prescribed, which can include oral medications or insulin therapy. Regular monitoring and follow-up with healthcare providers are essential to adjust treatment plans as needed.
Q8: What is the long-term outlook for someone with type 2 diabetes?
A: With effective management, many people with type 2 diabetes lead full and active lives. However, uncontrolled diabetes can lead to serious complications like heart disease, kidney damage, nerve issues, and vision problems. By staying informed and proactive, individuals can significantly reduce these risks and improve their overall health.
Q9: Where can someone find support and resources for managing type 2 diabetes?
A: Numerous resources are available for individuals with type 2 diabetes. Local healthcare providers, diabetes education centers, and support groups can provide valuable information and emotional support. Online resources, such as the American Diabetes Association, also offer guidance on managing the condition, as well as recipes and lifestyle tips.
Q10: What’s one final takeaway about living with type 2 diabetes?
A: The key takeaway is that type 2 diabetes is manageable. With the right knowledge, resources, and support, individuals can take control of their health, make informed decisions, and lead vibrant lives. Remember, small steps can lead to significant changes!
To Wrap It Up
As we draw the curtain on our exploration of type 2 diabetes, it’s clear that this condition is not merely a medical diagnosis but a multifaceted journey that intersects with lifestyle, nutrition, and individual resilience. Understanding the nuances of type 2 diabetes empowers us to navigate its challenges with informed choices and proactive measures. Whether through wholesome dietary adjustments, regular physical activity, or embracing ongoing support from healthcare professionals, each step taken can illuminate the path toward better health.
In a world where information is abundant yet often overwhelming, knowledge remains our greatest ally. By fostering awareness and encouraging dialogue, we can dismantle the stigmas surrounding diabetes and promote a culture of compassion and understanding. Remember, managing type 2 diabetes is not just about combating a disease; it’s about reclaiming vitality and embracing life in all its richness. So let’s continue to learn, share, and support one another on this journey—because together, we can turn the tide against diabetes and inspire a future where health and well-being are within everyone’s reach.