Understanding Pelvic Pain: Unraveling the Mystery Within
Pelvic pain is a complex and often misunderstood condition that affects countless individuals, transcending age, gender, and background. It can manifest as a sharp discomfort, a dull ache, or a persistent throb, and its origins can be as varied as the people who experience it. For some, pelvic pain may be an occasional nuisance, while for others, it becomes a daily struggle that impacts their quality of life. This article aims to explore the multifaceted nature of pelvic pain, delving into its potential causes, the emotional and psychological toll it can take, and the importance of seeking help. By shedding light on this often-taboo subject, we hope to empower those affected to understand their bodies better and navigate the path toward relief and healing. Join us as we unravel the mystery within and seek to demystify pelvic pain, one layer at a time.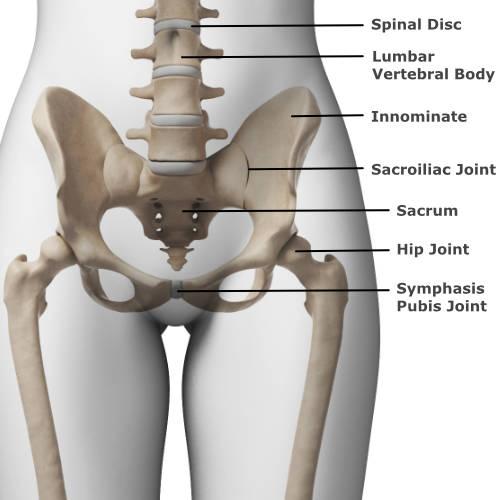
Understanding the Complex Causes of Pelvic Pain
Pelvic pain is a multifaceted issue that can stem from various underlying causes, making it a challenging condition to diagnose and treat. Factors contributing to this discomfort can range from musculoskeletal problems to reproductive health issues. Some common causes include:
- Endometriosis: A condition where tissue similar to the lining of the uterus grows outside it, often leading to severe pain.
- Pelvic inflammatory disease (PID): An infection of the female reproductive organs that can cause chronic pain.
- Interstitial cystitis: Chronic bladder condition that results in pelvic pain and frequent urination.
- Hernias: Occurs when tissue pushes through a weak spot in the abdominal muscles, leading to localized pain.
Additionally, psychological factors can exacerbate the perception of pain, making it essential to consider a holistic approach to treatment. Stress, anxiety, and depression may amplify feelings of discomfort, creating a vicious cycle. The interaction of these physical and emotional elements underscores the need for a thorough evaluation. Below is a simple comparison of potential sources of pelvic pain:
| Cause | Symptoms | Treatment Options |
|---|---|---|
| Endometriosis | Severe menstrual cramps, pain during intercourse | Hormonal therapy, surgery |
| PID | Pain in lower abdomen, fever | Antibiotics, surgery (in severe cases) |
| Interstitial Cystitis | Chronic pelvic pain, urinary urgency | Medications, bladder training |
| Hernia | Bulge in the groin area, pain during lifting | Surgery to repair the hernia |
Recognizing the Symptoms: When to Seek Help
Pelvic pain can manifest in various ways, and recognizing its symptoms is essential in determining whether you should seek professional assistance. Individuals may experience a range of sensations that can be alarming or concerning. Common symptoms to pay attention to include:
- Sharp or stabbing pain: Sudden, intense pain that can be debilitating.
- Dull ache: A persistent discomfort that may worsen with certain activities.
- Pain during intercourse: Discomfort or pain experienced during sexual activity.
- Changes in bowel or urinary habits: Increased frequency, urgency, or pain during these processes.
- Accompanying symptoms: Fever, nausea, or unexpected weight loss.
It’s crucial to listen to your body and understand the context of your pain. If you find that the discomfort is impacting your daily life or if you experience any of the following, it is advisable to consult with a healthcare professional:
- Severe pain: Pain that is unbearable or does not improve with over-the-counter medication.
- Persistent symptoms: Symptoms lasting more than a few days without improvement.
- Recurring episodes: Frequent occurrences of pelvic pain that disrupt your routine.
- Worsening condition: Any increase in severity or frequency of pain.
Diagnostic Approaches: Unraveling the Mystery of Pelvic Discomfort
Understanding the underlying causes of pelvic discomfort requires a multi-faceted diagnostic approach. Medical professionals often start with a thorough patient history and a detailed physical examination to gather insights into the nature of the pain. Key factors that may be explored include:
- Duration and frequency of pain episodes
- Location of discomfort—central, unilateral, or radiating
- Triggering factors, such as physical activity or dietary choices
- Associated symptoms, including urinary changes or gastrointestinal issues
Following the initial assessment, healthcare providers may recommend a combination of diagnostic tests to refine their understanding. These might include imaging techniques like ultrasounds or MRIs, which can reveal structural abnormalities, as well as laboratory tests to rule out infections or hormonal imbalances. The table below summarizes common diagnostic tools and their purposes:
| Diagnostic Tool | Purpose |
|---|---|
| Pelvic Ultrasound | To visualize reproductive organs and identify cysts or masses |
| MRI | To assess soft tissue structures and any pelvic floor abnormalities |
| Blood Tests | To check for infections, anemia, or hormonal issues |
| Laparoscopy | To directly view the pelvic organs for conditions like endometriosis |
Management Strategies: Practical Tips for Relief and Support
Managing pelvic pain can often feel overwhelming, but implementing effective strategies can make a significant difference. Consider incorporating the following approaches into your routine for relief and support:
- Exercise: Gentle activities like yoga or swimming can promote flexibility and reduce discomfort.
- Heat Therapy: Applying a heating pad or warm compress can help relax tense muscles and alleviate pain.
- Mindfulness and Relaxation: Techniques such as meditation or deep-breathing exercises can help manage stress and enhance pain tolerance.
- Dietary Adjustments: Keeping a food diary may help identify dietary triggers and promote a healthier gut, which can impact pelvic discomfort.
In addition to these self-care strategies, it may be beneficial to establish a support network, as sharing experiences can foster understanding and camaraderie. Consider these options:
- Support Groups: Joining a local or online group can provide emotional support and helpful resources.
- Professional Guidance: Consulting physical therapists or pain specialists can offer tailored treatment plans.
- Educational Resources: Seeking reliable information about pelvic pain can empower you and help you navigate your condition more effectively.
| Support Options | Benefits |
|---|---|
| Physical Therapy | Strengthens pelvic floor muscles |
| Cognitive Behavioral Therapy | Helps manage emotional responses to pain |
| Medication | Relieves pain and reduces inflammation |
The Role of Lifestyle Changes in Pelvic Pain Prevention
Making intentional lifestyle changes can significantly contribute to the prevention of pelvic pain. By focusing on a holistic approach that combines physical health, emotional well-being, and daily habits, individuals can create an environment conducive to long-term pelvic health. Key strategies include:
- Regular Exercise: Engaging in regular physical activity helps strengthen the pelvic floor muscles and improve overall body function.
- Balanced Diet: Consuming nutrient-rich foods supports bodily functions and can help reduce inflammation.
- Stress Management: Techniques such as yoga and meditation can alleviate tension that may contribute to pelvic pain.
- Hydration: Drinking ample water promotes healthy bodily functions and can prevent constipation, a common factor in pelvic discomfort.
In addition to these strategies, maintaining a healthy weight and avoiding prolonged periods of sitting can also play a crucial role in pelvic pain prevention. Regular check-ups with healthcare professionals can help identify any underlying issues early on. Consider the following preventive measures:
| Preventive Measure | Description |
|---|---|
| Strength Training | Enhances core stability and pelvic support. |
| Posture Correction | Improves alignment, reducing strain on pelvic structures. |
| Regular Stretching | Increases flexibility and relieves tension in pelvic muscles. |
Exploring Treatment Options: From Physical Therapy to Alternative Medicine
When dealing with pelvic pain, a variety of treatment options can provide relief and enhance overall well-being. Physical therapy is often one of the first lines of defense. Through targeted exercises and individualized care, physical therapists can help strengthen pelvic floor muscles, improve flexibility, and alleviate pain. Additionally, manual therapy techniques may be employed to release tension and improve blood flow in the pelvic region. Some common methods include:
- Myofascial release – targeting muscle and connective tissue
- Trigger point therapy – focusing on specific pain points
- Biofeedback - teaching control over pelvic floor muscles
In contrast, alternative medicine offers a holistic approach that can complement conventional treatments. Techniques such as acupuncture, yoga, and mindfulness meditation can play a significant role in managing symptoms. These therapies help reduce stress, promote relaxation, and improve one’s mental and emotional state, which is crucial for those suffering from chronic pain. Here’s a quick overview of some popular alternative therapies:
| Therapy | Benefits |
|---|---|
| Acupuncture | Reduces inflammation and promotes energy flow |
| Yoga | Enhances flexibility and strengthens core muscles |
| Mindfulness Meditation | Reduces stress and improves pain perception |
Q&A
Q&A on Pelvic Pain: Understanding Causes, Symptoms, and Treatments
Q1: What is pelvic pain, and how is it defined?
A1: Pelvic pain is a broad term that refers to discomfort in the lower abdominal area, typically below the belly button. It can be acute (short-term) or chronic (lasting more than six months) and may vary in intensity and nature—from sharp and stabbing to dull and achy. This type of pain can stem from various sources, making it a complex condition that often requires careful evaluation.
Q2: What are some common causes of pelvic pain?
A2: The causes of pelvic pain can be as diverse as the experiences of those who suffer from it. Common culprits include reproductive issues (like endometriosis and ovarian cysts), gastrointestinal problems (such as irritable bowel syndrome), urinary tract infections, and musculoskeletal issues. In some cases, the pain may stem from psychological factors, so it’s crucial to approach pelvic pain with a holistic perspective.
Q3: How can I recognize if my pelvic pain is serious?
A3: Pay attention to the characteristics of your pain. If you experience severe pain, sudden onset, or accompanying symptoms like fever, nausea, vomiting, or bleeding, it’s essential to seek medical attention promptly. Additionally, if the pain interferes with daily activities or worsens over time, don’t hesitate to consult a healthcare professional for further investigation.
Q4: What diagnostic tests are typically used to evaluate pelvic pain?
A4: Diagnosing pelvic pain often involves a combination of medical history, physical examinations, and imaging tests. Healthcare providers may recommend ultrasounds, CT scans, or MRIs to visualize the internal structures. Blood tests and laparoscopy (a minimally invasive surgical procedure) might also be used to gather more detailed information about the underlying causes.
Q5: What treatment options are available for pelvic pain?
A5: Treatment for pelvic pain varies based on its cause and severity. Options can include medication, such as pain relievers or hormonal therapies, physical therapy, lifestyle changes, and psychotherapy. In some cases, surgical interventions may be necessary to address underlying conditions. A multidisciplinary approach, involving gynecologists, gastroenterologists, and physical therapists, often yields the best results.
Q6: Are there any lifestyle changes that can help manage pelvic pain?
A6: Yes, adopting certain lifestyle changes can aid in managing pelvic pain. Regular exercise, a healthy diet, stress management techniques (like yoga or meditation), and proper hydration can all contribute to overall well-being and pain relief. Keeping a pain diary to track triggers and patterns may also help you and your healthcare provider formulate an effective management plan.
Q7: When should I seek help for pelvic pain?
A7: It’s wise to seek help if you notice persistent or severe pelvic pain, especially if it disrupts your daily life or is accompanied by other concerning symptoms. Early intervention is key in identifying potential issues and determining the most effective treatment strategy. Remember, you are not alone, and help is available to guide you through this journey.
Q8: Is pelvic pain common, and who is most affected?
A8: Pelvic pain is relatively common and does not discriminate—it can affect individuals of all ages and backgrounds. However, women are more likely to experience certain types of pelvic pain due to reproductive health issues. Awareness and education about pelvic pain can empower those affected to seek help and foster open discussions about their symptoms.
Understanding pelvic pain is a vital step toward effective management. By exploring its causes, recognizing symptoms, and seeking appropriate treatment, individuals can take proactive steps in reclaiming their well-being.
To Wrap It Up
pelvic pain is a complex and multifaceted issue that affects many individuals, transcending age, gender, and lifestyle. As we’ve explored, its origins can range from the benign to the more serious, and understanding the underlying causes is crucial for effective management and treatment. Whether it manifests as a fleeting discomfort or a chronic condition, it is essential to approach pelvic pain with compassion and awareness.
If you or someone you know is grappling with this condition, remember that seeking professional guidance is the first step towards relief and recovery. Knowledge is power, and by fostering open conversations about pelvic health, we can break down the stigmas that often surround these intimate issues. As we continue to learn and share, may we cultivate a supportive community where individuals feel empowered to address their concerns and find the care they deserve. After all, a healthy body and mind begin with understanding oneself.