Understanding Chronic Constipation: Unraveling the Mystery of a Common Digestive Dilemma
In the intricate tapestry of human health, the digestive system often plays a pivotal role, weaving together the threads of nutrition, energy, and well-being. Yet, for many, this essential network can become ensnared in the frustrating grip of chronic constipation—a condition that transcends occasional discomfort to become a persistent and often misunderstood challenge. While it is a common ailment, affecting millions around the globe, chronic constipation remains shrouded in stigma and confusion. In this article, we will delve into the nuances of this condition, exploring its potential causes, symptoms, and the myriad of strategies available for relief. By shedding light on this often-ignored aspect of health, we aim to empower individuals with knowledge and foster a deeper understanding of the importance of digestive wellness in our daily lives. Join us as we embark on a journey to demystify chronic constipation and discover pathways to improved digestive health.
Understanding the Complex Causes of Chronic Constipation
Chronic constipation can arise from a variety of interrelated factors, which complicates its management and treatment. One key component is dietary habits. A diet low in fiber, often lacking fruits, vegetables, and whole grains, can significantly slow down digestive processes. Additionally, inadequate fluid intake can lead to harder stools, making them difficult to pass. Beyond diet, lifestyle choices play a crucial role. Sedentary behavior, stress, and irregular bathroom habits can disrupt the natural rhythm of bowel movements. Understanding these elements is critical in addressing chronic constipation effectively.
Moreover, underlying medical conditions can contribute significantly to this issue. Conditions such as hypothyroidism, diabetes, and irritable bowel syndrome (IBS) often affect bowel function. Medications, particularly those used for pain management or antidepressants, may have constipation as a side effect, further complicating the situation. It is also important to consider psychological factors; anxiety and depression can lead to disrupted bowel function. The interplay of these causes creates a complex web that requires a holistic approach to treatment, encompassing dietary adjustments, lifestyle changes, and potential medical interventions.
Recognizing the Symptoms Beyond the Obvious
While many people associate chronic constipation with the inability to have regular bowel movements, the symptoms can extend far beyond the bathroom. Often, individuals may experience a range of *subtle but significant* signs that can affect their overall well-being. These may include:
- Abdominal discomfort: A feeling of fullness or bloating that can impact daily activities.
- Fatigue: Chronic feelings of tiredness that may stem from the body’s struggle to eliminate waste effectively.
- Loss of appetite: An aversion to food, which can be a direct consequence of gastrointestinal distress.
- Mood changes: Increased irritability or anxiety that can surface due to ongoing discomfort associated with constipation.
Additionally, some individuals may notice physical manifestations of their condition that are often overlooked. These can include:
- Skin issues: Eruptions or a dull complexion may indicate a body in distress, struggling to detoxify properly.
- Back pain: A recurring ache in the lower back, which can be tied to the strain of constipation on the body’s systems.
- Headaches: Frequent headaches that appear without clear triggers, possibly linked to dehydration or dietary irregularities.
Dietary Changes That Can Alleviate Constipation
Making thoughtful dietary changes can significantly improve digestive health and help alleviate chronic constipation. Fiber-rich foods play a crucial role in promoting regular bowel movements by adding bulk to the stool. Incorporating a variety of whole grains, fruits, and vegetables into your diet can make a noticeable difference. Some excellent choices include:
- Leafy greens: Spinach, kale, and collard greens provide essential nutrients and fiber.
- Fruits: Apples, pears, and berries are not only delicious but are also high in fiber.
- Legumes: Beans, lentils, and chickpeas are fantastic sources of both protein and fiber.
Moreover, staying hydrated is vital for maintaining healthy digestion. Increased fluid intake can soften the stool and make it easier to pass. Aim for at least eight glasses of water a day, and consider incorporating hydrating foods into your meals, such as cucumbers, watermelon, and oranges. Additionally, limiting processed foods and reducing the intake of dairy products can further help mitigate constipation. Here’s a simple table to outline some beneficial food categories:
| Food Category | Examples |
|---|---|
| Whole Grains | Oats, brown rice, quinoa |
| Fruits | Bananas, prunes, figs |
| Vegetables | Carrots, broccoli, sweet potatoes |
The Role of Hydration in Digestive Health
Staying adequately hydrated plays a pivotal role in maintaining optimal digestive function. Water helps to dissolve nutrients and soluble fibers, making it easier for the body to absorb essential vitamins and minerals. Additionally, hydration softens stool, increasing its bulk and promoting smoother passage through the intestines. Without sufficient water intake, the digestive system can become sluggish, leading to discomfort and conditions such as chronic constipation. It is essential to recognize the symptoms of dehydration, which can include fatigue, dry mouth, and infrequent bowel movements.
To enhance hydration and support digestive health, consider incorporating the following strategies into your daily routine:
- Drink water regularly: Aim for at least 8 glasses per day, adjusting based on physical activity and climate.
- Consume hydrating foods: Incorporate fruits and vegetables with high water content, such as cucumbers, watermelon, and oranges.
- Limit dehydrating beverages: Reduce intake of caffeine and alcohol, which can contribute to dehydration.
Tracking your water intake can be beneficial. Below is a simple table to help you monitor your daily hydration levels:
| Day | Water Intake (Glasses) |
|---|---|
| Monday | 8 |
| Tuesday | 7 |
| Wednesday | 10 |
| Thursday | 6 |
| Friday | 9 |
Effective Lifestyle Modifications for Long-Term Relief
Making thoughtful lifestyle changes can significantly enhance your digestive health and provide long-term relief from chronic constipation. Start by incorporating more fiber-rich foods into your daily diet, such as fruits, vegetables, whole grains, and legumes. Fiber adds bulk to your stool, making it easier to pass. Aim for a daily intake of at least 25-30 grams of fiber. Staying adequately hydrated is equally important; drink plenty of water throughout the day to help soften your stool. Consider establishing a routine around your bathroom visits—try to set aside a few minutes each day for a relaxed attempt to use the toilet, preferably after meals when the digestive system is most active.
In addition to dietary adjustments, regular physical activity can play a crucial role in alleviating constipation. Aim for at least 30 minutes of moderate exercise most days of the week. This can include walking, cycling, or yoga, all of which can stimulate bowel movement. It’s also beneficial to manage stress levels through relaxation techniques like meditation or deep breathing exercises, as stress can negatively impact your digestive health. Keeping a consistent daily schedule, including regular sleep patterns, can further support your body’s natural rhythms and promote healthy digestion.
When to Seek Professional Help for Chronic Constipation
Chronic constipation can significantly impact your quality of life, and recognizing when it’s time to seek professional guidance is crucial. If you’ve been experiencing infrequent bowel movements, generally fewer than three times a week, or if you find yourself straining excessively, it’s advisable to consult a healthcare provider. Additional symptoms that warrant a visit to a medical professional include:
- Severe abdominal pain
- Blood in your stool
- Unexplained weight loss
- Persistent nausea or vomiting
- Change in bowel habits lasting more than three weeks
It’s also important to seek help if lifestyle changes and over-the-counter remedies fail to alleviate your symptoms after a reasonable period. A healthcare professional can help identify underlying conditions, such as irritable bowel syndrome or even more serious gastrointestinal disorders. They can also provide tailored treatment plans that may include:
| Treatment Options | Description |
|---|---|
| Dietary Modifications | Increased fiber intake through fruits, vegetables, and whole grains. |
| Laxatives | Over-the-counter or prescription options for immediate relief. |
| Biofeedback Therapy | Techniques to improve bowel function through enhanced awareness. |
| Medications | Prescription medications that stimulate bowel movement. |
Q&A
Q&A: Understanding Chronic Constipation
Q: What is chronic constipation?
A: Chronic constipation is a condition characterized by infrequent bowel movements or difficulty passing stool that persists for several weeks or longer. While occasional constipation is common, chronic cases can significantly impact daily life and overall health, leading to discomfort and distress.
Q: How can I tell if I have chronic constipation?
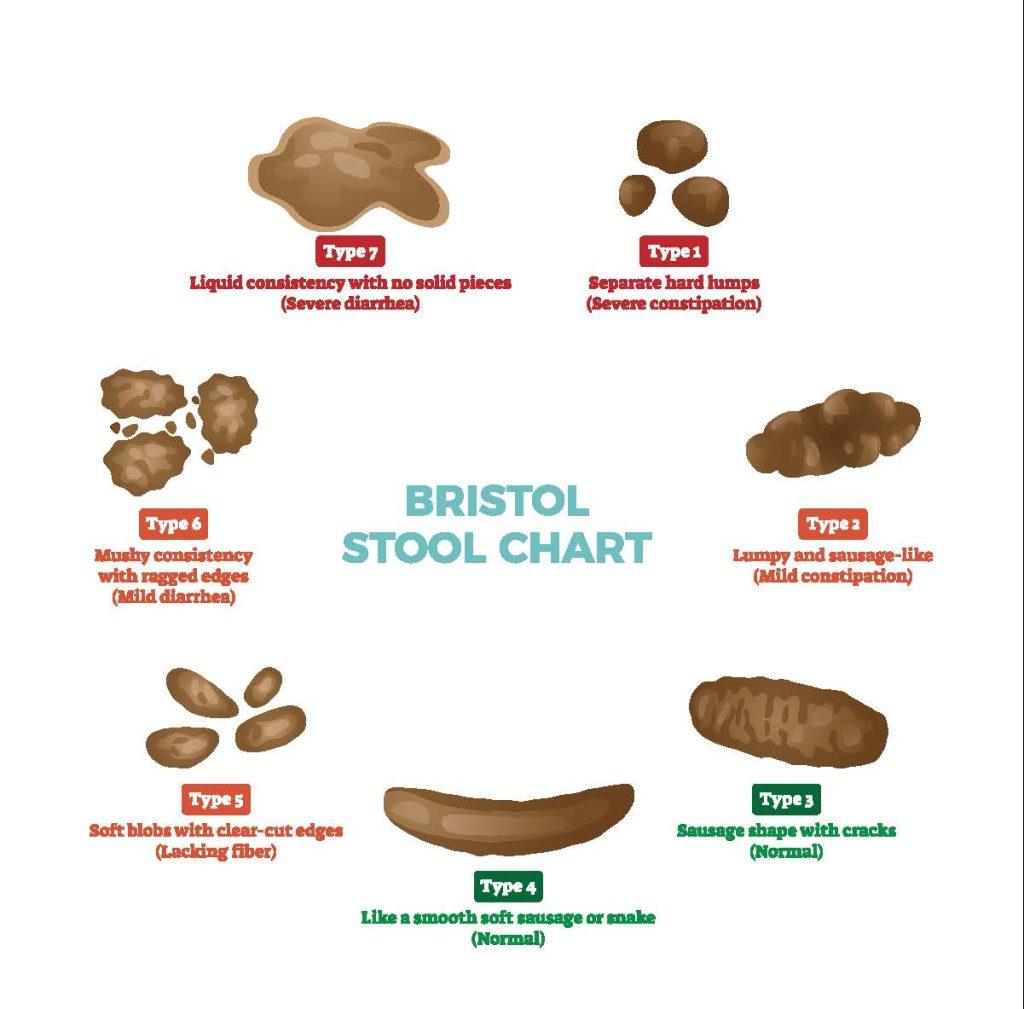
A: If you experience fewer than three bowel movements a week, straining during defecation, or a sensation of incomplete evacuation consistently over several weeks, it may indicate chronic constipation. Other signs to watch for include hard or lumpy stools and abdominal pain.
Q: What causes chronic constipation?
A: Chronic constipation can arise from various factors including poor diet, lack of physical activity, dehydration, certain medications, and underlying health conditions such as irritable bowel syndrome (IBS) or hypothyroidism. Psychological factors, including stress and anxiety, can also play a role.
Q: Are there risk factors for developing chronic constipation?
A: Yes, several risk factors can increase the likelihood of developing chronic constipation. These include age (it’s more common in older adults), a diet low in fiber, sedentary lifestyle, certain medications (like opioids), and specific health conditions that affect digestive function.
Q: How can I manage chronic constipation?
A: Management often involves lifestyle modifications such as increasing dietary fiber (fruits, vegetables, whole grains), drinking plenty of water, regular physical activity, and establishing a routine for bowel movements. Additionally, over-the-counter laxatives or prescription medications may be recommended by healthcare professionals.
Q: When should I see a doctor about chronic constipation?
A: It’s advisable to seek medical attention if you experience severe abdominal pain, persistent constipation lasting more than three weeks, blood in your stool, or if you notice significant changes in your bowel habits. These could indicate a more serious underlying condition.
Q: Can chronic constipation lead to complications?
A: Yes, chronic constipation can lead to various complications, such as hemorrhoids, anal fissures, or fecal impaction. In severe cases, it may contribute to rectal prolapse or other gastrointestinal issues, emphasizing the importance of addressing the condition promptly.
Q: Are there any natural remedies for chronic constipation?
A: Many people find relief from chronic constipation through natural remedies such as increasing fiber intake, using probiotics, and consuming natural laxatives like prunes. Staying hydrated and engaging in regular exercise can also help promote healthy bowel movements.
Q: Is chronic constipation a sign of something more serious?
A: While chronic constipation is often manageable with lifestyle changes, it can occasionally be a symptom of a more serious condition, such as colorectal cancer or metabolic disorders. It’s important to consult a healthcare provider if symptoms are severe or persistent.
Q: How can I prevent chronic constipation?
A: Prevention strategies include maintaining a balanced diet rich in fiber, staying hydrated, exercising regularly, and not ignoring the urge to have a bowel movement. Establishing a consistent daily routine for meals and bathroom visits can also be beneficial in promoting regularity.
This Q&A aims to shed light on the often-overlooked topic of chronic constipation, providing clear answers to common questions while encouraging proactive health management.
In Conclusion
chronic constipation is much more than just an occasional discomfort; it is a complex condition that can significantly impact one’s quality of life. By understanding the underlying causes, recognizing the symptoms, and exploring the various treatment options available, individuals can take proactive steps to reclaim their digestive health. Whether through dietary adjustments, lifestyle changes, or medical interventions, finding the right approach is crucial. Remember, you are not alone in this journey—there are resources, support, and solutions waiting to be discovered. As we move forward, let’s cultivate a deeper awareness about digestive wellness, encourage open conversations, and foster a community that prioritizes health. After all, when it comes to our well-being, every little step counts.