Unlocking the Rhythm of Life: An Exploration of Ovulation
In the intricate dance of human reproduction, ovulation stands as a pivotal moment, a silent yet powerful player in the symphony of fertility. Each month, under the influence of hormones and biological rhythms, a woman’s body prepares for the possibility of new life. This remarkable process, often shrouded in mystery, not only holds the key to conception but also offers insights into broader aspects of health and well-being. From the flutter of a developing follicle to the potential for a new beginning, understanding ovulation is essential for anyone looking to navigate the nuances of their reproductive journey. In this article, we will delve into the science behind ovulation, its phases, and its significance, unraveling the threads that connect biology, health, and the miracle of life.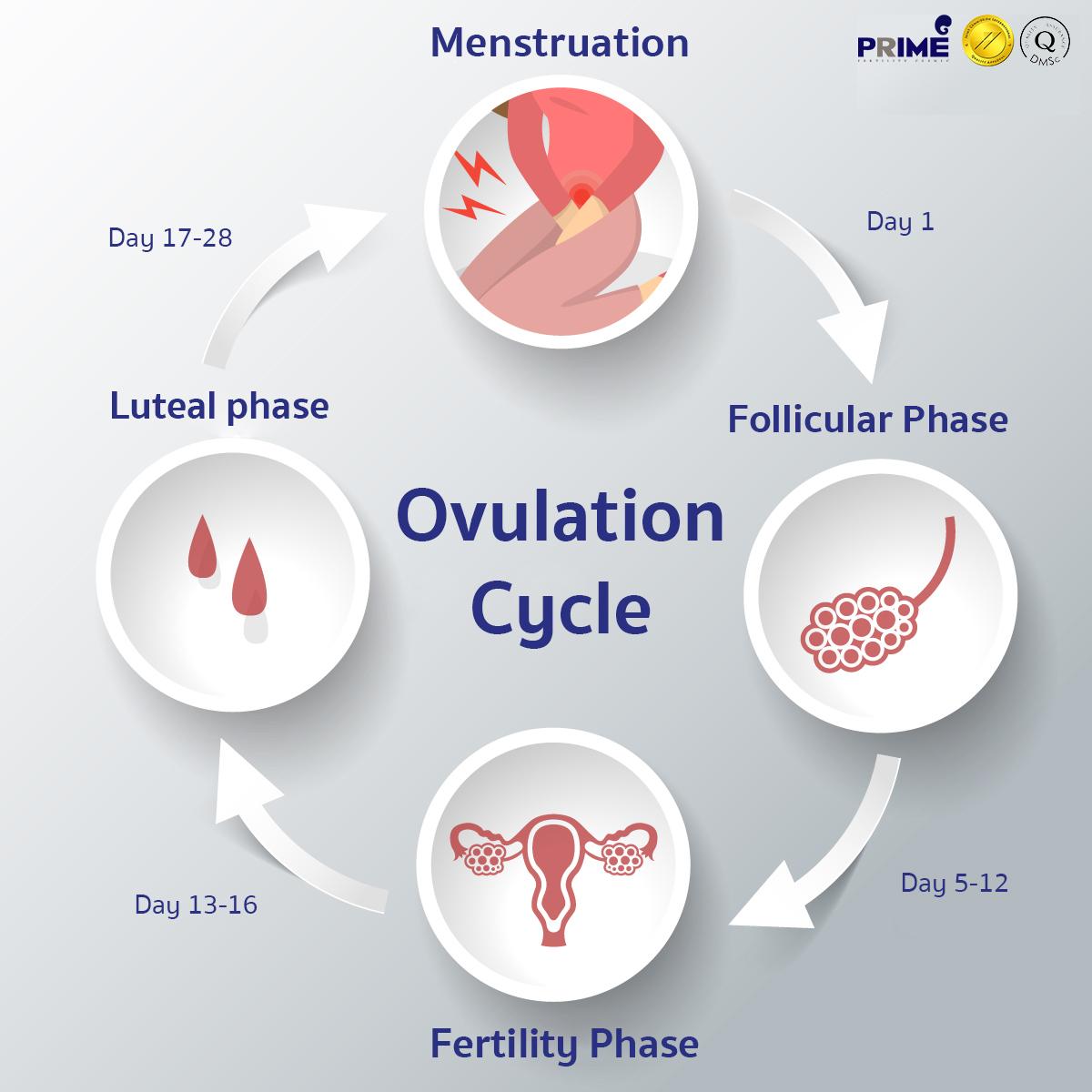
Understanding the Ovulation Cycle and Its Phases
The ovulation cycle is a remarkable process that plays a crucial role in a woman’s reproductive health. It typically lasts around 28 days but can vary between 21 to 35 days. This cycle is divided into several key phases, each characterized by specific physiological changes. Understanding these phases can empower individuals to manage their reproductive health more effectively. The main phases include:
- Menstrual Phase: The shedding of the uterine lining occurs, leading to menstrual bleeding.
- Follicular Phase: Hormones stimulate the growth of follicles in the ovaries, with one follicle eventually maturing into an egg.
- Ovulation: The mature follicle releases an egg, typically around day 14 of a 28-day cycle.
- Luteal Phase: After ovulation, the empty follicle transforms into the corpus luteum, which produces hormones to prepare the uterus for potential pregnancy.
During ovulation, many women experience physical and emotional symptoms due to hormonal fluctuations. These can include changes in cervical mucus, heightened libido, and slight cramping. Monitoring these signs can be beneficial for those trying to conceive or practicing natural family planning. The following table summarizes these symptoms and their timing within the cycle:
| Symptom | Timing |
|---|---|
| Cervical Mucus Changes | Days 12-16 |
| Increased Libido | Day 14 |
| Cramping | Day 14 |
| Breast Tenderness | Days 21-24 |
The Role of Hormones in Ovulation: A Deep Dive
Hormones play a pivotal role in the intricate process of ovulation, orchestrating a symphony of biological events that culminate in the release of an egg from the ovaries. The primary hormones involved include luteinizing hormone (LH), follicle-stimulating hormone (FSH), estrogen, and progesterone. These hormones are secreted by the pituitary gland and the ovaries in a carefully timed sequence. As the follicle matures, FSH stimulates growth and estrogen production, which heightens the sensitivity of the pituitary gland to produce a surge of LH. This surge is what ultimately triggers ovulation, marking a critical phase in a woman’s menstrual cycle that prepares the body for potential fertilization.
Moreover, the hormonal interplay continues post-ovulation, influencing the next stages of the cycle. Following the release of the egg, the remnants of the follicle transform into the corpus luteum, which secretes progesterone. This hormone is essential for preparing the uterine lining for a potential pregnancy. If fertilization does not occur, progesterone levels drop, leading to menstruation. The delicate balance of these hormones is crucial, as any disruption can lead to irregular ovulation or fertility issues. Understanding this hormonal dance not only sheds light on the biological underpinnings of ovulation but also emphasizes the importance of hormonal health in reproductive processes.
| Hormone | Function |
|---|---|
| Follicle-Stimulating Hormone (FSH) | Stimulates follicle growth and estrogen production |
| Luteinizing Hormone (LH) | Triggers ovulation and corpus luteum formation |
| Estrogen | Regulates the menstrual cycle and prepares the uterine lining |
| Progesterone | Prepares the uterine lining for possible implantation |
Identifying Signs of Ovulation: What to Watch For
Understanding the signs of ovulation can empower you to track your fertility more effectively. Here are some key indicators to watch for:
- Change in Cervical Mucus: As ovulation approaches, you may notice an increase in clear, stretchy mucus that resembles raw egg whites. This is a sign that your body is preparing for potential conception.
- Basal Body Temperature (BBT) Shift: A slight increase in your BBT, typically around 0.5 to 1 degree Fahrenheit, can indicate that ovulation has occurred. Tracking your temperature daily can provide valuable insights.
- Ovulation Pain: Some individuals experience mild cramping or discomfort on one side of the abdomen during ovulation, known as mittelschmerz.
- Heightened Libido: Many women report an increase in sexual desire during ovulation, driven by hormonal changes.
It can also be helpful to observe the timing of these signs in relation to your menstrual cycle. Below is a simple table outlining the average cycle phases and associated signs:
| Cycle Phase | Typical Duration | Signs to Observe |
|---|---|---|
| Follicular Phase | Day 1-13 | Low BBT, thick cervical mucus |
| Ovulation | Day 14 | Clear mucus, BBT spike, ovulation pain |
| Luteal Phase | Day 15-28 | Rise in BBT, potential PMS symptoms |
Nutritional Strategies to Support Healthy Ovulation
To cultivate a robust ovulatory cycle, it is essential to focus on a well-rounded and nutrient-dense diet. Certain nutrients play a pivotal role in hormonal balance and the overall reproductive health of women. Key nutrients to incorporate include:
- Omega-3 Fatty Acids: Found in fish like salmon and flaxseeds, these healthy fats help reduce inflammation and support hormone production.
- Vitamin D: Often referred to as the ‘sunshine vitamin,’ it is crucial for regulating menstrual cycles. Sources include sunlight, fortified foods, and fatty fish.
- Folate: This B vitamin is vital for DNA synthesis and can be found in leafy greens, legumes, and citrus fruits.
- Iron: Important for ovulatory function, iron can be obtained from red meat, spinach, and lentils.
Additionally, maintaining a healthy body weight is vital for optimal ovulation. Excessive weight can disrupt hormonal balance, while being underweight can also hinder ovulatory function. Incorporating a well-structured meal plan that includes:
| Food Group | Examples |
|---|---|
| Proteins | Lean meats, fish, beans |
| Healthy Fats | Nuts, seeds, avocados |
| Whole Grains | Quinoa, brown rice, oats |
| Fruits & Vegetables | Berries, broccoli, sweet potatoes |
By prioritizing these nutritional strategies, you can create an environment that supports healthy ovulation and enhances overall reproductive health.
Common Challenges in Ovulation and How to Address Them
Understanding the intricacies of ovulation can sometimes be overshadowed by various challenges that individuals may face. One significant issue is irregular menstrual cycles, which can make it difficult to predict ovulation. Factors such as stress, weight fluctuations, and hormonal imbalances can contribute to this irregularity. By maintaining a healthy lifestyle that includes a balanced diet and regular exercise, individuals can help regulate their cycles. Additionally, tracking ovulation through methods such as basal body temperature or ovulation predictor kits can provide more clarity and assist in family planning.
Another common obstacle is ovulation disorders, which may stem from conditions like polycystic ovary syndrome (PCOS) or thyroid dysfunction. These disorders can hinder the release of eggs, complicating conception efforts. Seeking professional medical advice is crucial for diagnosis and management. Treatments may include hormonal therapies, lifestyle modifications, or medications like Clomiphene citrate to stimulate ovulation. Below is a brief overview of some common disorders and potential treatments:
| Disorder | Treatment Options |
|---|---|
| Polycystic Ovary Syndrome (PCOS) |
|
| Hypothyroidism |
|
Maximizing Fertility: Tips for Timing and Tracking Ovulation
Understanding your menstrual cycle is crucial for enhancing your chances of conception. Ovulation typically occurs around the midpoint of your cycle, but individual cycles can vary. To pinpoint this vital window, consider tracking various indicators of ovulation. Basal Body Temperature (BBT) is one method, as your temperature rises slightly after ovulation due to hormonal changes. You can also observe changes in cervical mucus; around ovulation, it becomes clear, stretchy, and resembles raw egg whites, signaling peak fertility. Keeping a calendar or using an app can help you visualize patterns and predict your ovulation days more accurately.
In addition to tracking bodily changes, timing intercourse strategically is essential. Aim to have sex during the fertile window, which spans the five days leading up to ovulation and the day of ovulation itself. This increases the likelihood of sperm meeting the egg. To assist in planning, here’s a simple table outlining the fertile days based on a typical 28-day cycle:
| Cycle Day | Fertile Status |
|---|---|
| 1-5 | Low Fertility |
| 6-10 | Increasing Fertility |
| 11-14 | High Fertility |
| 15-20 | Decreasing Fertility |
| 21-28 | Low Fertility |
Incorporate these methods into your routine to maximize your fertility potential. Don’t forget that lifestyle factors like stress, nutrition, and exercise also play a pivotal role in reproductive health, so nurturing your overall well-being can further support your journey toward conception.
Q&A
Q&A on Ovulation: Understanding the Rhythm of Reproductive Health
Q1: What is ovulation, and why is it important?
A: Ovulation is a pivotal phase in the menstrual cycle where an ovary releases a mature egg, making it available for fertilization. This natural event typically occurs around the midpoint of the cycle, usually 14 days before the start of menstruation. Understanding ovulation is essential for those trying to conceive, as it marks the window of peak fertility. Additionally, insights into ovulation can help in monitoring reproductive health and understanding menstrual irregularities.
Q2: How can someone tell when they are ovulating?
A: There are several signs that can indicate ovulation is approaching. Some common indicators include changes in cervical mucus—which becomes clearer and more stretchy, resembling egg whites—as well as a slight increase in basal body temperature. Some may also experience mild abdominal pain known as mittelschmerz. Additionally, ovulation predictor kits can detect hormonal changes in urine, providing a more precise indication of when ovulation occurs.
Q3: How long does ovulation last?
A: The actual event of ovulation is quite brief, lasting around 24 hours. However, the fertile window, during which conception is possible, spans about six days: the five days leading up to ovulation and the day of ovulation itself. Sperm can survive in the female reproductive tract for up to five days, making this period crucial for those seeking to become pregnant.
Q4: Can factors like stress or illness affect ovulation?
A: Absolutely. Ovulation can be influenced by various external factors, including stress, illness, significant weight changes, and hormonal imbalances. Stress can disrupt the hypothalamus, which regulates hormonal signals necessary for ovulation. Similarly, conditions like polycystic ovary syndrome (PCOS) can lead to irregular ovulation. Keeping track of lifestyle factors and menstrual patterns can provide valuable insights into reproductive health.
Q5: What should someone do if they suspect they have ovulation issues?
A: If someone suspects they have irregular ovulation or experiences significant changes in their menstrual cycles, consulting a healthcare provider is advisable. A doctor can conduct evaluations, including hormone testing and ultrasounds, to determine the underlying cause. They can also suggest lifestyle modifications or treatments to help regulate ovulation and support reproductive goals.
Q6: Is it possible to ovulate without having a period?
A: Yes, it is possible to ovulate without experiencing a menstrual period. This can occur in cases such as amenorrhea (the absence of menstruation) or during certain life stages like breastfeeding. Women with irregular cycles might also ovulate sporadically. Tracking other signs of ovulation can help in these situations, even if periods are absent.
Q7: How does age affect ovulation?
A: Age plays a significant role in a woman’s ovulation patterns and overall fertility. As women age, especially after the age of 35, the quality and quantity of eggs decline, leading to irregular ovulation and increased chances of infertility. It’s essential to understand these changes and seek guidance if planning for a family later in life.
Q8: Are there any myths about ovulation worth dispelling?
A: Certainly! One common myth is that ovulation always occurs on the same day each month, but cycle length can vary significantly among individuals. Another misconception is that once a woman has a child, her ovulation will always be regular, which isn’t necessarily true. Educating oneself about ovulation can help debunk these myths and promote a better understanding of reproductive health.
—
This creative Q&A aims to clarify the nuances of ovulation while providing reliable information for readers interested in learning more about this essential aspect of reproductive health.
Key Takeaways
In the intricate dance of life, ovulation plays a pivotal role, a silent conductor guiding the symphony of reproduction. Understanding this biological rhythm not only empowers us with knowledge about our bodies but also enriches our appreciation for the marvels of nature. As we draw the curtain on our exploration of ovulation, let us carry forward the insights gleaned—from the hormonal fluctuations to the signs that signal its approach. Whether you’re planning for a family or simply curious about the cycles that govern our existence, awareness of ovulation is a step toward embracing the complexities of fertility and health. So, as we close this chapter, may you continue to seek understanding and celebrate the remarkable processes that define life itself.